Abstract
Background:Lower extremity trauma during earthquakes accounts for the largest burden of geophysical disaster-related injuries. Insufficient pain management is common in disaster settings, and regional anesthesia (RA) has the potential to reduce pain in injured patients beyond current standards. To date, no prospective research has evaluated the use of RA in a disaster setting. This cross-sectional study assesses knowledge translation and skill acquisition outcomes for lower extremity RA performed with and without ultrasound guidance among a cohort of Médecins Sans Frontières (MSF) volunteers who will function as proceduralists in a planned randomized controlled trial evaluating the efficacy of RA for pain management in an earthquake setting.
Methods:Generalist humanitarian healthcare responders, including both physicians and nurses, were trained in ultrasound guided femoral nerve block (USGFNB) and landmark guided fascia iliaca compartment block (LGFICB) techniques using didactic sessions and interactive simulations during a one-day focused course. Outcome measures evaluated interval knowledge attainment and technical proficiency in performing the RA procedures. Knowledge attainment was assessed via pre- and post-test evaluations and procedural proficiency was evaluated through monitored simulations, with performance of critical actions graded by two independent observers.
Results:Twelve humanitarian response providers were enrolled and completed the trainings and assessments. Knowledge scores significantly increased from a mean pre-test score of 79% to post-test score of 88% (p<0.001). In practical evaluation of the LGFICB, participants correctly performed a median of 15.0 (Interquartile Range (IQR) 14.0-16.0) out of 16 critical actions. For the USGFNB, the median score was also 15.0 (IQR 14.0-16.0) out of 16 critical actions. Inter-rater reliability for completion of critical actions was excellent, with inter-rater agreement of 83.3% and 91.7% for the LGFICB and USGFNB evaluations, respectively.
Discussion:Prior to conducting a trial of RA in a disaster setting, providers need to gain understanding and skills necessary to perform the interventions. This evaluation demonstrated attainment of high knowledge and technical skill scores in both physicians and nurses after a brief training in regional anesthesia techniques. This study demonstrates the feasibility of rapidly training generalist humanitarian responders to provide both LGFICB and USGFNB during humanitarian emergencies.
Funding Statement
Funding for this study was provided by a Research for Health in Humanitarian Crises (R2HC) grant administered by Enhancing Learning and Research for Humanitarian Assistance (ELRHA). The funding agency had no role in the design of the study.Notice of Correction
6 February 2017: PLOS Currents – Correction: Aluisio AR, Teicher C, Wiskel T, Guy A, Levine A. Focused Training for Humanitarian Responders in Regional Anesthesia Techniques for a Planned Randomized Controlled Trial in a Disaster Setting. PLOS Currents Disasters. 2016 Nov 16 . Edition 1. doi: 10.1371/currents.dis.e75f9f9d977ac8adededb381e3948a04. View Correction.
Background
Between 1994 and 2013, approximately 7000 natural disasters were reported, affecting more than 200 million people and accounting for over one million deaths globally. Among geophysical disasters, earthquakes result in high mortality rates and account for the largest burden of injuries1,2. Research from multiple settings demonstrates that earthquake-associated trauma most commonly causes injuries to the lower extremities3,4,5,6. Inadequate pain management during natural disasters, where resources are often constrained, is common and can result in both short-term and long-term physiologic and psychological sequela among an already high-risk patient population7,8,9,10.
Prior studies have demonstrated that regional anesthesia (RA) is a rapid and safe method for reducing pain caused by lower extremity trauma, and as such may have a role in improving pain management during the acute response phase of a major earthquake11,12,13,14,15. However, most studies on RA have been conducted in high-resource settings by specially trained proceduralists and have only enrolled patients with simple hip or femur fractures, which may not be generalizable to the more complex injury pattern typical of earthquake-related trauma16,17,18. There are anecdotal reports of the use of both landmark guided (LG) and US-guided (USG) RA for treatment of earthquake-related injuries, suggesting feasibility in the use of these modalities in disaster settings9,19,20. However, there have been no high-quality studies conducted evaluating the effectiveness, safety, or acceptability of RA in the aftermath of a major earthquake.
The Regional Anesthesia for Painful Injuries after Disasters (RAPID) study is randomized controlled trial (RCT) that will be carried out in the immediate aftermath of a major earthquake to determine whether RA provided by generalist humanitarian medical responders, either with or without ultrasound-guidance, can improve pain treatment for lower limb injuries, above current standards of care21. The RAPID study will be implemented by Médecins Sans Frontières (MSF) personnel deployed in response to an earthquake in a low- or middle-income countries (LMIC) setting21,22,23. Limited prior research on training non-specialist providers in RA in pre-hospital and emergency department settings has demonstrated successful skill attainment24,25,26,27. Although this evidence supports the concept of generalist humanitarian providers being capable of performing RA, no data exists pertaining specifically to this population, who provide care in unique practice environments. This study assesses knowledge translation and skill acquisition for simulated lower extremity RA performed both with and without ultrasound guidance by a cohort of MSF association members and describes the focused training methodology used.
Methods
Ethics
The RAPID study has received ethical approval from the Médecins Sans Frontières Ethical Review Board (Reference number: 1524) and has been preregistered at ClinicalTrials.gov (number: NCT02698228)21. All training participants provided written informed consent for study activities which were conducted in accordance with the Declaration of Helsinki.
Study Design Setting and Population
This cross-sectional study was designed to evaluate the efficacy of a focused training in regional anesthesia for lower extremity injuries provided to MSF volunteers who will serve as research proceduralists in a future RCT of RA for pain management in earthquake victims21. Study activities were carried out during a one-day training in June of 2015 at the MSF-USA office (New York City, United States).
The study population was comprised of physician and nurse responders who had previously been deployed to humanitarian emergencies and were members of the MSF-USA association. Participants were made aware of the RAPID study and training prior to the meeting via digital correspondence with study investigators and were solicited to volunteer for participation.
Participant Training and Assessment
Training activities were designed to provide understanding of RA principles and competence in performing landmark guided fascia iliaca compartment blocks (LGFICB) and ultrasound-guided femoral nerve blocks (USGFNB). Study throughput is outlined in Figure 1. Participants completed a baseline knowledge assessment prior to the provision of training activities. The pre-assessment was comprised of fifteen multiple-choice questions that covered topics pertaining to techniques for general RA and specifically to LGFICB and USGFNB. Training and assessment materials were derived from joint committee recommendations for education and training in ultrasound-guided interventional pain procedures from American, European and Australasian international pain and anesthesia societies28. Participants were randomly allocated to take one of two versions of the assessment exam (test A or test B), with each exam having fifteen questions which were unique in both query stems and possible responses but which covered the same content matter and key concepts.
Following the initial assessment, participants took part in a three-hour interactive didactic session lead by study investigators using a semi-structured discussion platform that allowed for open-form content exchange between all participants. The educational information focused on RA principles and specific methodologies in performing LGFICB and USGFNB28. Additional information relating to the RAPID study protocols was also provided. Given the evidence supporting the use of simulation in teaching invasive procedures29, participants took part in three simulation-based training sessions subsequent to the didactic session. These three sessions focused on performance of USGFNB, LGFICB and general ultrasound-guided needle injection. The duration of each practical session was 45 minutes, with a 3:1 participant to instructor ratio in each session. All instructors were board certified physicians in either anesthesia or emergency medicine or senior emergency medicine residents with experience in RA techniques. The LGFICB sessions were taught using a live model simulation with a focus on surface anatomy and technical aspects specific to the procedure. For the USGFNB sessions, a femoral regional anesthesia ultrasound model (CAE Healthcare™, model number: BPF1400) was used, focusing on technical aspects of the procedure specific to perineural anesthetic delivery. For the ultrasound-guided needle injection training, regional anesthesia ultrasound training block models (CAE Healthcare™, model number: BPNP150) were used and participants were able to perform multiple injections and practice needle control and delivery under ultrasound guidance with instructor support. All ultrasound trainings and evaluations were performed using Sonosite Edge™ and Terason uSmart™ 3200T ultrasound machines with high-frequency 6-13MHz linear transducers.
After completion of training activities, each participant was assessed through two observed simulation exams for performance of the LGFICB and the USGFNB. In each exam, participants were asked to perform the RA techniques using standard clinical equipment and a femoral regional anesthesia ultrasound model (CAE Healthcare™, model number: BPF1400). During the simulation exams, two independent reviewers assessed each participant’s technical competency using a preformed critical actions checklist with an objective scoring system. Assessed parameters evaluated appropriate positioning; identification of anatomic and ultrasonographic landmarks; use of sterile technique; provision of local superficial anesthetic; needle delivery; anesthetic injection; and proper procedural monitoring for possible adverse events.
A post-training, fifteen question multiple-choice exam was performed to assess interval knowledge attainment. In the post-training assessment, participants were crossed-over to complete the alternative exam to the one they took at baseline (i.e., those initially allocated to test A completed test B and those which started with test B completed test A).
Data Collection Outcome Measures
Baseline data on participants was collected using a structured questionnaire. Information on demographics, healthcare training, humanitarian response activities, ultrasound and RA experience was gathered. Knowledge assessment exams were scored with a single best answer for each question and participants were assigned a percent correct for both the pre-test and post-test. During observed simulation exams for the RA techniques, each rater provided a critical action completion score ranging from zero to sixteen based on eight assessment parameters. Accrued data was de-identified and entered into a password-protected database that was accessible only by study personnel.
The primary outcome measures were the change in knowledge attainment based on mean pre- and post-test scores on the standardized exams and demonstration of technical competency in performing the LGFICB and USGFNB RA techniques. Technical competency was assessed based on adequate performance of critical actions during simulation assessments. Secondary outcome measures included the inter-rater reliability for the standardized critical action checklist and separate subgroup analyses of physician and nurses.
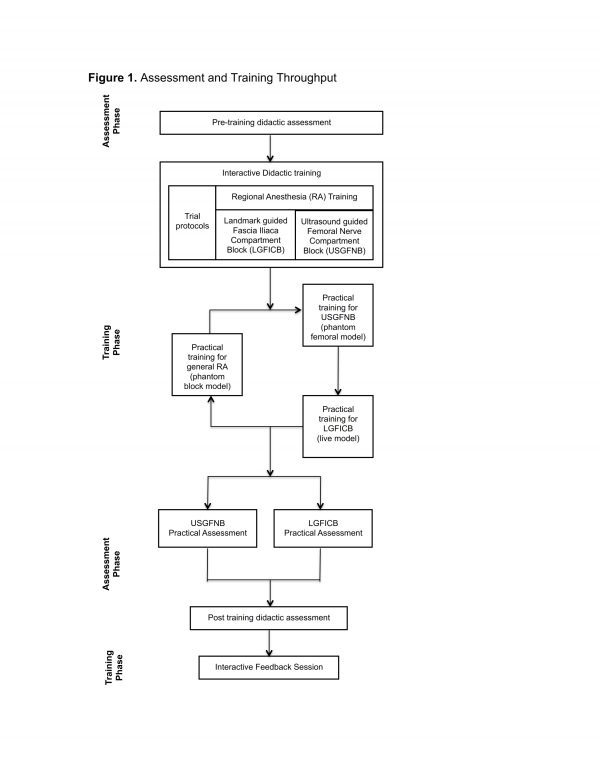
Fig. 1: Assessment and Training Throughput
Statistical Analysis
Statistical analyses were performed using STATA 13.0 (StataCorp LP, College Station, USA). Characteristics of the cohort were evaluated using descriptive methods. Categorical variables were explored using frequencies with percentages, and continuous variables were analyzed using medians with corresponding interquartile ranges (IQR) or means with associated 95% confidence intervals (95% CI). Given the small sample size knowledge attainment data was analyzed using Shapiro-Wilks tests and frequency distributions to evaluate for normality. The results were found to satisfy criteria for normality and as such, one sample paired t-tests were used for the primary outcome of change in mean knowledge scores. A p value less than 0.05 was considered significant in primary outcome assessments.
Median scores with IQR for each rater were calculated for the LGFICB and USGFNB simulation assessments. Inter-rater reliability (IRR) was evaluated across all critical assessment variables based on rater agreement derived using Cohen’s kappa calculation. Kappa values were interpreted according to previously utilized criteria with agreement classified as greater than 0.80 as representing excellent IRR30,31. Stemming from inherent difference in healthcare training and practice roles, outcomes for the cohort were stratified and analyzed based on participants’ professional training as a nurse or physician. Subgroups were compared using independent sample t tests or Mann-Whitney U tests for normally and non-normally distributed variables respectively. To account for multiple testing, a Bonferroni correction was utilized and a significance level of less than 0.008 was used for stratified analyses32.
Results
Twelve MSF association members were enrolled and all participants completed the full study training and assessment procedures. The median age of the cohort was 41 years and the majority of participants were female. Half of participants reported their primary healthcare training as nurse and half as physician. The median years of healthcare practice and humanitarian response experience were eleven and five years respectively. Half of the cohort had prior experience with ultrasound use, though only a minority reported previous clinical application of RA techniques (Table 1).
* MSF abbreviates Médecins San Frontières
Characteristics
n (%) / Median (IQR)
Age (years)
41 (35, 48)
Sex
Male
2 (16.7%)
Female
10 (83.3%)
Primary healthcare training
Nures
6 (50.0%)
Medical Doctor
6 (50.0%)
Duration providing healthcare (years)
11 (10, 21)
Duration as MSF* response personnel (years)
5 (3, 9)
Number of response missions performed with MSF*
4 (4, 7)
Prior clinical use of ultrasound
No
6 (50.0%)
Yes
6 (50.0%)
Prior clinical use of regional anesthesia
No
10 (83.3%)
Yes
2 (16.7%)
The primary study outcomes are summarized in Table 2. Training activities resulted in a significant increase in mean knowledge assessment scores of 9.2% (p<0.001). The mean pre-training and post-training scores were 79.2% and 88.4%, respectively. Median values for achieved critical actions during simulation assessments were all greater than or equal to 15 as scored by the independent raters. Overall an excellent degree of IRR was observed between rater evaluations for the simulated RA assessments. The IRR agreement for technical assessments of the LGFICB and USGFNB were 83.3% and 91.7% respectively (Table 2).
* Values represent the percent mean score with associated 95% confidence intervals (95% CI), # LGFICB abbreviates landmark guided fascia iliaca block and USGFNB abbreviates ultrasound guided femoral nerve block, † Reported as median score with associated interquartile range (IQR) out of possible score of sixteen required critical actions
Pre-training
Post-training
Percent Change
p
Didactic Knowledge assessment score*
79.2 (73.9-84.4)
88.4 (82.3-94.2)
9.2%
<0.001
Rater 1†
Rater 2†
Kappa
–
LGFICB assessment#
15.0 (14.0, 16.0)
15.0 (15.0, 16.0)
0.83
–
USGFNB assessment#
15.0 (14.0, 16.0)
15.5 (14.5, 16.0)
0.92
–
Table 3 demonstrates stratified outcome assessments based on participants’ healthcare training. There were no significant differences identified in knowledge attainment or technical skill performance between the physician and nurse subgroups.
* Values represent the percent mean score with associated 95% confidence intervals (95% CI), # LGFICB abbreviates landmark guided fascia iliaca block and USGFNB abbreviates ultrasound guided femoral nerve block, † Reported as median score with associated interquartile range (IQR), maximum possible score out of sixteen required critical actions
Assessment Type
Nurse
Physician
p
Pre-training didactic exam*
78.7 (74.3-83.1)
79.6 (67.6-91.7)
0.86
Post training didactic exam*
91.7 (85.6-97.8)
85.2 (73.7-96.1)
0.23
LGFICB assessment#
Rater 1†
14.5 (14.0, 15.0)
14.0 (14.0, 16.0)
0.18
Rater 2†
15.0 (14.0, 16.0)
15.0 (15.0, 16.0)
0.06
USGFNB assessment#
Rater 1†
15.5 (15.0, 16.0)
14.0 (14.5, 16.0)
0.35
Rater 2†
15.5 (14.0, 16.0)
15.5 (15.0, 16.0)
0.80
Discussion
This study assessed knowledge translation and skill acquisition outcomes for simulated lower extremity RA performed both with and without ultrasound guidance among a small cohort of MSF volunteers who will function as proceduralists in a planned randomized controlled trial that will assess the efficacy of RA for pain management in the acute phase of a major earthquake21. The results demonstrate high knowledge and technical skill acquisition with good agreement between independent raters. These findings illustrate success of the focused training methods used in this population of response providers in gaining proficiency in both LGFICB and USGFNB regional anesthesia.
In the acute response phase to a natural disaster, where resources are often constrained, oligoanalgesia is common7,8,9. Standard pain management in disaster settings for severe lower limb injuries focuses on the use of parenteral narcotic medications33,34. However, such medications are frequently unavailable creating preexistent barriers to analgesic treatment in low-income disaster settings35,36. Additionally, even when narcotic medications are accessible patients with trauma often have tenuous hemodynamic states, making administration of narcotics clinically unfavorable, especially in situations where continuous cardiorespiratory monitoring and personnel are limited. Subsequently, insufficient pain management can potentiate both short-term and long-term sequela, including immunosuppression, thrombotic complications, posttraumatic stress disorders, and chronic pain syndromes, further increasing the morbidity associated with the index injuries8,10. Anecdotal reports and recent review articles have suggested that regional anesthesia has the potential to improve pain control in disaster settings9,10,19,20,37. However, the published literature on the use of RA in disasters is limited, and to date no randomized controlled trial has evaluated the efficacy, safety and acceptability of nerve blocks in a disaster context. The planned RAPID study will address these specific gaps in the research21. A key step in executing the trial is appropriately training personnel to carry out the procedures and protocols. This study provides evidence of success in personnel training for a small cohort of generalist humanitarian responders to perform RA.
Standardized assessment and training in research procedures is important in reducing error and deriving valid trial results38. The present study used rigorous methodologies that integrated both interactive didactic sessions and multimodal simulation to train providers in focused RA. The employed training principles are similar to prior documented works in procedural skills and RA training that have utilized systematic assessments of technical skills39,40. Additionally, the assessment methods for technical competency in evaluating procedural abilities were checklist-based, which have been shown to result in more thorough and objective assessments of component skills in multi-step medical procedures41,42. Furthermore, the assessment outcomes for procedural performance, evaluated by independent raters, overall demonstrated excellent agreement, supporting validity in the results31,43. These findings, in conjunction with the significant improvement in interval didactic assessment scores in both the full cohort and individual professional sub-groups, support the efficacy of the training methodology.
Although prior studies have assessed the performance of femoral never blockades after brief trainings in emergency department settings among physician and nurse trainees this study is the first to evaluate formal training of generalist humanitarian response providers in RA methods24,25,44,45. In addition, a prehospital study of pain management for lower extremity injuries performed by emergency medical service providers found that approximately 89% of patients had effective analgesic treatment with provision of prehospital RA26. This prehospital efficacy was replicated in a cohort of paramedic proceduralists employing fascia iliaca compartment blocks in a controlled trial among patients with femur fractures27. The congruent findings in successful RA techniques between the prehospital and hospital based studies and the present work supports validity in the findings and bolsters the feasibility of pre-training generalist providers to perform RA in an acute disaster setting.
This work must be interpreted in the context of certain limitations. The presented results illustrate short-term acquisition of knowledge and skills among the MSF volunteers trained, but do not allow for assessment of application in actual disaster situations, nor for evaluation of skill retention over time. It is likely that similar to most technical skill sets, the study proceduralists will require refresher training prior to execution of the RAPID study, which has been built into the trial design. Although the population of humanitarian responders was drawn from a large pool of MSF volunteer personnel, the cohort was relatively small and not randomly selected, and as such the generalizability of these outcomes to the greater population of disaster healthcare personnel is not certain. During completion of the RAPID study this will be partially addressed, as there will be further onsite training for locally recruited healthcare providers, who will also serve as proceduralists during the later study phases. These later phase providers will be trained and assessed onsite using the same methods as described in this report.
Prior to conducting a trial of RA in a disaster setting, providers need to gain the knowledge and skills necessary to perform the interventions. This study demonstrated high knowledge and technical skills scores with excellent inter-rater agreement between independent evaluators, illustrating the success of the focused training for generalist humanitarian response providers in the selected RA techniques. This work, in conjunction with the planned RAPID study, will contribute to the development of an enhanced evidence base to guide future care and improve health outcomes among high-risk patients injured in the settings of humanitarian emergencies.
Data Availability Statement
The data used for this analysis can be accessed via: https://figshare.com/s/1825267cbf21863b6cf4.
Competing Interests
All authors declare that they have no competing interests to disclose.
Corresponding Author
Adam R. Aluisio, MD, MSc
Warren Alpert School of Medicine, Brown University, Department of Emergency Medicine
55 Claverick Street, Room 274
Providence, Rhode Island 02912, USA
Email: [email protected]
Appendices: Abbreviations
CRED: Centre for Research on the Epidemiology of Disasters
FICB: Fascia iliaca compartment block
FNB: Femoral nerve block
IQR: Interquartile Range
IRR: Inter-rater reliability
LG: Landmark guided
LGFICB: Landmark guided fascia iliaca compartment block
LMIC: low- and middle-income countries
MoH: Ministry of Health
MSF: Médecins Sans Frontières
RA: Regional anesthesia
RCT: Randomized Controlled Trial
SAE: Serious Adverse Events
SD: Standard Deviation
US: Ultrasound
USG: Ultrasound guided
USGFNB: Ultrasound guided femoral nerve block
WHO: World Health Organization
References
- Guha-Sapir D, Vos T. Earthquakes, an Epidemiological Perspective on Patterns and Trends. In: Human Casualties in Earthquakes: Progress in Modelling and Mitigation. New York, New York: Springer, 2011., 13-24.
- Centre for Research on the Epidemiology of Disasters. The Human cost of Natural Disasters 2015, A Global Perspective. Accessed 2 April 2016: https://reliefweb.int/sites/reliefweb.int/files/resources/PAND_report.pdf.
- Jacquet GA, Hansoti B, Vu A, Bayram JD. Earthquake-related injuries in the pediatric population: a systematic review. PLoS currents. 2013;5.
- Mulvey JM, Awan SU, Qadri AA, Maqsood MA. Profile of injuries arising from the 2005 Kashmir earthquake: the first 72 h. Injury. May 2008;39(5):554-560.
- Carlson LC, Hirshon JM, Calvello EJ, Pollak AN. Operative care after the Haiti 2010 earthquake: implications for post-disaster definitive care. The American journal of emergency medicine. Feb 2013;31(2):429-431.
- Kang P, Zhang L, Liang W, et al. Medical evacuation management and clinical characteristics of 3,255 inpatients after the 2010 Yushu earthquake in China. The journal of trauma and acute care surgery. Jun 2012;72(6):1626-1633.
- Chen G, Lai W, Liu F, et al. The dragon strikes: lessons from the Wenchuan earthquake. Anesthesia and analgesia. Mar 1 2010;110(3):908-915.
- Sinatra R. Causes and consequences of inadequate management of acute pain. Pain medicine. Dec 2010;11(12):1859-1871.
- Missair A, Gebhard R, Pierre E, et al. Surgery under extreme conditions in the aftermath of the 2010 Haiti earthquake: the importance of regional anesthesia. Prehospital and disaster medicine. Nov-Dec 2010;25(6):487-493.
- Lippert SC, Nagdev A, Stone MB, Herring A, Norris R. Pain control in disaster settings: a role for ultrasound-guided nerve blocks. Annals of emergency medicine. Jun 2013;61(6):690-696.
- Antonis MS, Chandwani D, McQuillen K. Ultrasound-guided placement of femoral 3-in-1 anesthetic nerve block for hip fractures. Academic Emergency Medicine. 2006; 13: S122-3.
- Marhofer P, Schrogendorfer K, Koinig H, Kapral S, Weinstable C, Mayer N. Ultrasoundographic guidance improves sensory block and onset time of three-in-one blocks. Anesthesia and Analgesia. 1997; 85:854-7.
- Snoeck MM, Vree TB, Gielen MJ, Lagerwert AJ. Steady state bupivacaine plasma concentrations and safety of a femoral “3-in-1” nerve block with bupivacaine in patients over 80 years of age. International Journal of Clinical Pharmacology and Therapeutics. 2003; 41:107-13.
- McGlone R, Sadhra K, Hamer DW, Pritty PE. Femoral nerve block in the initial management of femoral shaft fractures. Archives of emergency medicine. Sep 1987;4(3):163-168.
- Tan TT, Coleman MM. Femoral blockade for fractured neck of femur in the emergency department. Annals of emergency medicine. Oct 2003;42(4):596-597; author reply 597.
- Foss NB, Kristensen BB, Bundgaard M, et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology. Apr 2007;106(4):773-778.
- Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. Jun 2013;20(6):584-591.
- Christos SC, Chiampas G, Offman R, Rifenburg R. Ultrasound-guided three-in-one nerve block for femur fractures. The western journal of emergency medicine. Sep 2010;11(4):310-313.
- Rice MJ, Gwertzman A, Finley T, Morey TE. Anesthetic practice in Haiti after the 2010 earthquake. Anesthesia and analgesia. Dec 2010;111(6):1445-1449.
- Shah S, Dalal A, Smith RM, Joseph G, Rogers S, Dyer GS. Impact of portable ultrasound in trauma care after the Haitian earthquake of 2010. The American journal of emergency medicine. Oct 2010;28(8):970-971.
- Regional Anaesthesia for Painful Injuries After Disasters. Registration number: NCT02698228. Accessed 2 April 2016: https://clinicaltrials.gov/ct2/show/NCT02698228
- The World Bank. How we classify countries. Accessed 2 April 2016: https://data.worldbank.org/about/country-classifications.
- WHO Collaborating Centre for Research on the Epidemiology of Disasters. EM-DAT: the OFDA/CRED International Disasters Data Base 2004. Brussels, Belgium. 2004.
- Haines L, Dickman E, Ayvazyan S, et al. Ultrasound-guided fascia iliaca compartment block for hip fractures in the emergency department. J Emerg Med. Oct 2012;43(4):692-697.
- Akhtar S, Hwang U, Dickman E, Nelson BP, Morrison RS, Todd KH. A brief educational intervention is effective in teaching the femoral nerve block procedure to first-year emergency medicine residents. J Emerg Med. Nov 2013;45(5):726-730.
- Dochez E, van Geffen GJ, Bruhn J, Hoogerwerf N, van de Pas H, Scheffer G. Prehospital administered fascia iliaca compartment block by emergency medical service nurses, a feasibility study. Scandinavian journal of trauma, resuscitation and emergency medicine. 2014;22:38.
- McRae PJ, Bendall JC, Madigan V, Middleton PM. Paramedic-performed Fascia Iliaca Compartment Block for Femoral Fractures: A Controlled Trial. The Journal of emergency medicine. May 2015;48(5):581-589.
- Narouze SN, Provenzano D, Peng P, et al. The American Society of Regional Anesthesia and Pain Medicine, the European Society of Regional Anaesthesia and Pain Therapy, and the Asian Australasian Federation of Pain Societies Joint Committee recommendations for education and training in ultrasound-guided interventional pain procedures. Regional anesthesia and pain medicine. Nov-Dec 2012;37(6):657-664.
- Huang GC, McSparron JI, Balk EM, et al. Procedural instruction in invasive bedside procedures: a systematic review and meta-analysis of effective teaching approaches. BMJ quality & safety. Nov 5 2015.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. Mar 1977;33(1):159-174
- McHugh ML. Interrater reliability: the kappa statistic. Biochemia medica. 2012;22(3):276-282.
- Streiner DL. Best (but oft-forgotten) practices: the multiple problems of multiplicity-whether and how to correct for many statistical tests. The American journal of clinical nutrition. Oct 2015;102(4):721-728.
- Médecins Sans Frontières. Clinical guidelines Diagnosis and treatment manual 2013 Edition. ISBN 2-906498-86-6. Accessed 2 April 2016: https://refbooks.msf.org/msf_docs/en/clinical_guide/cg_en.pdf.
- Walter Reed Army Medical Center. The Military Advanced Regional Anesthesia and Analgesia Handbook “Acute Pain Management in the Field”. Washington, DC. 2008: 95-101. Accessed 2 April 2016: https://www.dvcipm.org/clinical-resources/dvcipm-maraa-book-project.
- Manjiani D, Paul DB, Kunnumpurath S, Kaye AD, Vadivelu N. Availability and utilization of opioids for pain management: global issues. The Ochsner journal. Summer 2014;14(2):208-215.
- International Narcotics Control Board. Availability of Internationally Controlled Drugs: Ensuring Adequate Access for Medical and Scientific Purposes Indispensable, adequately available and not unduly restricted. United Nations Publication: New York, New York 2016. Accessed 2 April 2016:https://www.incb.org/documents/Publications/AnnualReports/AR2015/English/Supplement-AR15_availability_English.pdf.
- Park CL, Roberts DE, Aldington DJ, Moore RA. Prehospital analgesia: systematic review of evidence. J R Army Med Corps. Dec 2010;156(4 Suppl 1):295-300.
- Mitchell M, Jolley J. Research Design Explained, Eighth Edition. Belmont, California: Wadsworth, 2013., 165-167.
- Aggarwal R, Grantcharov TP, Darzi A. Framework for systematic training and assessment of technical skills. Journal of the American College of Surgeons. Apr 2007;204(4):697-705.
- Smith HM, Kopp SL, Jacob AK, Torsher LC, Hebl JR. Designing and implementing a comprehensive learner-centered regional anesthesia curriculum. Regional anesthesia and pain medicine. Mar-Apr 2009;34(2):88-94.
- Lammers RL, Davenport M, Korley F, et al. Teaching and assessing procedural skills using simulation: metrics and methodology. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. Nov 2008;15(11):1079-1087.
- Rosenthal R, Gantert WA, Hamel C, et al. Assessment of construct validity of a virtual reality laparoscopy simulator. Journal of laparoendoscopic & advanced surgical techniques. Part A. Aug 2007;17(4):407-413.
- Hallgren KA. Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutorials in quantitative methods for psychology. 2012;8(1):23-34.
- Fletcher AK, Rigby AS, Heyes FL. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: a randomized, controlled trial. Ann Emerg Med. Feb 2003;41(2):227-233.
- Randall A, Grigg L, Obideyi A, Srikantharajah I. Fascia Iliaca compartment block: A nurse-led initiative for preoperative pain management in patients with a fractured neck of femur. Journal of Orthopaedic Nursing 2008;12:69-74.

Leave a Comment
You must be logged in to post a comment.