Methods: We focused on four steps: #1: Appraising the emergency management research portfolio of VHA-based researchers; #2: Obtaining systematic information on VHA’s role in emergency management and the healthcare needs of veterans during disasters; #3: Based upon gaps between the current research portfolio and the existing evidence base, identifying strategic priorities using a research agenda-setting conference; and #4: Laying the groundwork to foster the conduct of emergency management research within VHA.
Results: Identified research priorities included how to prevent and treat behavioral health problems related to a disaster, the efficacy of training programs, crisis communication strategies, workforce resilience, and evacuating veterans from health care facilities.
Conclusion: VHA is uniquely situated to answer research questions that cannot be readily addressed in other settings. VHA should partner with other governmental and private entities to build on existing work and establish shared research priorities.
]]>Introduction
In addition to providing healthcare for veterans, the United States Veterans Health Administration (VHA), part of the Department of Veterans Affairs (VA), is charged with improving the Nation’s preparedness for response to war, terrorism, national emergencies, and natural disasters by developing plans and taking actions to ensure continued service to veterans, as well as supporting national, state, and local emergency management, public health, safety and homeland security efforts.1,2,3 Under the National Response Framework of the United States (U.S.), VHA has support responsibility under 7 of the 15 Emergency Support Functions including emergency management, public health, and medical services. Consequently, VHA has directly provided care for veterans—and sometimes non-veterans—during every major national disaster since 1992.
By law, VHA provides health care to enrolled Veterans first, but can provide support to communities when there are local emergency needs or federally declared disasters. In this capacity, VA’s extensive resources as the largest integrated healthcare delivery system in the U.S. (more than 350,000 personnel at more than 1,300 medical sites serving about 9 million Veterans) may be used to support other Federal and state agencies and local communities by providing public health and medical services following emergencies and disasters. For example, VA deployed more than 1,300 personnel and 12 mobile clinics to Louisiana and Mississippi following Hurricane Katrina; the clinics provided care to about 15,000 patients, including 11,000 who were not Veterans. The VA also provide significant amounts of care to individuals impacted by events as diverse as the World Trade Center attacks on September 11, 2001,4 and the earthquake in Haiti that occurred in 2010. VA staff regularly participate in emergency planning for events such as domestic Olympics, Presidential Inaugurations, and Papal visits.
In mid-2008, VHA’s Office of Public Health (OPH, now part of the VHA Office of Patient Care Services) provided funding to researchers at the Health Services Research & Development (HSR&D) Center of Excellence for the Study of Healthcare Provider Behavior to develop a plan to establish a comprehensive, VHA emergency management research and program evaluation agenda. It was hoped that the agenda would provide a basis for fostering the conduct of more VHA-based emergency management research, and, over time, position VHA as a national leader in emergency management research. This paper summarizes the process and outcomes of this effort, and outlines VHA’s research and evaluation priorities.
VHA Emergency Management Research Agenda-Setting Process
Emergency management professionals and researchers with significant funded or published research on emergency preparedness were invited to join a conference wherein attendees would assist in the creation of a research agenda designed to address gaps in research on VHA emergency management. The planning group operated within the framework of a four-step action plan adapted from Yano and colleagues (2006)5 for a VHA Women’s Health Research Agenda-Setting Conference (Table 1).
Action Plan
Approach
Step #1: Critically appraise the VHA emergency management research portfolio
1. Obtain and review history of emergency management funding to VHA researchers; 2. Analyze data by funding source (e.g., VHA, other federal, private, foundation)
Step #2: Obtain systematic information about VHA emergency management to provide an evidence base for the research agenda
Conduct a systematic VHA emergency management literature review, including review of grey literature as well as peer-reviewed literature
Step #3: Based on gaps between the current VHA research portfolio (step #1) and the assessment of the evidence base (step #2), identify priorities for a VHA emergency management research agenda
1. Review and adapt priority-setting strategies by other agencies (e.g., Department of Defense, Centers for Disease Control and Prevention); 2. Review VHA strategic plans3. Conduct gap analysis, priority setting, and consensus development during a VHA emergency-management research agenda setting conference (held July 2009)
Step #4: Foster the conduct of VHA emergency management research
1. Build research capacity through collaboration, networking, and mentoring; 2. Increase awareness and visibility of VHA emergency management research
Appraisal of VHA’s Research Portfolio
To support strategic planning, it was necessary to assess the current state of existing emergency management research within VHA. This historical research portfolio provides a foundation for the reader to understand both the nature and scope of the then current VA emergency management research portfolio upon which the conference planning and subsequent research agenda were based. The following section reviews emergency management research funding secured by VHA researchers through 2008.
Emergency Management Funding
During 2003-2008, VHA researchers based at one of the HSR&D Centers of Excellence were funded by HSR&D and the VHA Office of Mental Health Services, and non-VHA sources, including the Agency for Healthcare Research and Quality (AHRQ), the Centers for Disease Control and Prevention (CDC), and the National Institutes of Health (NIH) (Table 2).
Fiscal Year
VHA
Non-VHA
Total
2003
$354,279
$131,500
$485,764
2004
$441,336
$851,859
$1,293,195
2005
$489,235
$466,395
$955,630
2006
$523,910
$958,709
$1,482,619
2007
$385,896
$598,982
$984,878
2008
$0
$1,370,472
$1,370,472
Total Number of Studies: 6
Total Number of Studies: 11
VHA-funded emergency management research increased steadily from 2003 to 2006, then decreased by more than 25% in 2007. No VHA researchers were funded by VHA to conduct emergency management research during 2008. Non-VHA funding increased more than sixfold from 2003 to 2004, then decreased by about half the following year. From 2006 to 2008, non-VHA funding to VHA researchers who study emergency management continued to fluctuate. Some of the fluctuation in funding from year to year during this time period may be due to the cyclical nature of funding related to the occurrence of major disasters. For example, it is likely that the increase in funding for emergency management research in 2005 and 2006 was a response to Hurricanes Katrina and Rita.
It is evident from this review that emergency management is an emerging area of research in terms of VHA funding. As shown in Table 3, emergency management funding has remained relatively constant at under one percent of total funding to VHA researchers based at HSR&D Centers of Excellence. In comparison, former emerging VHA research topics such as women veterans’ health started at approximately 2-3% of total funding to VHA researchers.5 Subsequent to the VHA Women’s Health Research Agenda-Setting Conference in 2004, women’s health was identified as a VHA research priority, leading to an increase in funding for women veterans’ health research.
Emergency management research funding
Total research funding
% of Total
2005
$955,630
$160,750,113
0.6%
2006
$1,482,619
$156,282,076
0.9%
2007
$984,878
$165,994,469
0.6%
2008
$1,370,472
$170,103,121
0.8%
In summary, the total amount of emergency management research funding secured by VHA researchers stayed relatively constant from FY 2004 to FY 2008, although VHA funding declined to zero in FY 2008. Non-VHA funding decreased in FY 2005, but increased again beginning in FY 2006. VHA funding comprised 34%-73% of the total funding VHA emergency management researchers secured from FY 2003 to FY 2007. NIH was the primary sponsor of this type of research during FY 2007 and FY 2008.
The number of VHA-based researchers funded by VHA sources increased from 9 during FY 2003 to a high of 27 in FY 2007, before declining to zero during FY 2008. In contrast, the number of VHA-based researchers funded by non-VHA sources increased from 1 during FY 2003 to a high of 6 during FY 2007, before dropping to 3 during FY 2008.
The decline in VHA funding in FY 2008 in part reflects the small number of studies in progress during this time period, and suggests a need for more consistent funding in this area in order to attract and grow the emergency management research community within VHA. These trends suggest a clear interest among the VHA community for conducting research in the area of emergency management, but one that is limited by cyclical factors such as variations in funding over time.
Establishing the Evidence Base for Agenda Development
Research Portfolio
A review of HSR&D-funded studies provides a broad overview of emergency management issues confronting VHA. A systematic search within VHA databases identified six HSR&D-funded studies since 2002. One of the six studies focused on surveillance, two on education, and three on the response to bioterrorism or natural disasters (two of which focused on vulnerable populations).
Summary of HSR&D Studies
The six HSR&D-funded studies since 2002 are limited in scale and scope (Table 4). The one surveillance study points to the importance and usefulness of automated monitoring of electronic health information in early illness detection. The two educational studies, involving providers and patients, indicate an existing need to adapt educational interventions to the VHA population. Of the three response studies, two evaluated actual events and one involved scenario-modeling. Collectively, they addressed VHA’s ability to compare responses across locations and time, the ability to study vulnerable populations, and the recognition of VHA as a potential target due its governmental affiliation.
PI
Background
Objective
Methods
Findings
S. Delisle(IIR 06-119)
Early detection is critical for infectious disease outbreaks of public health importance. Disease surveillance can be potentially enhanced through automated monitoring of electronic medical records compared to manual case reporting systems
To automate the use of data from VHA’s computerized patient record system (CPRS) to enhance outbreak detection by including illness progression and severity to reduce “noise” of common syndromes
Clinical data was grouped by respiratory disease severity using diagnostic and procedures notes, laboratory results, and free text of clinical notes
Automated surveillance for influenza should integrate information from prescriptions and free text clinical notes. Case detection with emergency medical records focusing on influenza-like cases with fever can reduce delay and workload to detect influenza epidemics
C. I. Kiefe(BTI 02-092)
The VHA medical system can play an essential role following a biological terrorist attack or infectious outbreak due to its extensive record in disaster preparedness
To develop and test web-based teaching modules to increase VHA clinicians’ knowledge about biological warfare agents
Web-based educational intervention was tested at 15 VHA facilities via a randomized controlled trial with 332 participants
The VHA program demonstrated higher anthrax, but not smallpox, post- training provider knowledge than the information offered on the CDC’s website
M. Sano(BTI 02-233)
Limited efforts to prepare general public for a bioterrorism incident have been conducted
To develop educational materials for veterans about bioterrorism; to provide coping mechanisms for getting though a bioterrorism incident; to evaluate methods for material delivery
A Veterans’ Survey on Bio-Terrorism (VSOB) (the initial and a follow up) was mailed to 2923 veterans
VSOB, the first instrument to evaluate veterans’ knowledge, attitudes, beliefs, anxiety and educational needs connected to bioterrorism, was developed
A. Dobalian(RRP 06-134)
Existing research within and outside of VHA does not sufficiently address health issues for mentally ill and/or frail veterans during evacuations
To understand evacuation and response in VHA nursing homes after Hurricanes Katrina and Rita
Data were collected via 13 semi-structured interviews with organizational representatives at 4 VHA medical centers and two representatives at the regional level
Administrators primarily relied on local resources, prior experience and local planning rather than on state and federal response systems in their response to the hurricanes. Despite significant difficulties during patient evacuation, VHA response was generally perceived as positive. Retaining staff and a viable organization during and after a disaster presented a difficulty. Respondents reported unaddressed preparedness needs even more than one year post-disaster
F. M. Weaver(RRP 06-135)
Individuals with spinal cord injuries and disorders are at particular risk during disasters due to impaired mobility and special needs, such as power wheelchairs and ventilator dependency
To use identified lessons learned from natural disasters that impacted veterans with spinal cord injuries and disorders (SCI&D) in developing a toolkit, which focuses on enhancing natural disaster preparedness for facilities caring for veterans with SCI&D
Thirty interviews were conducted (16 with providers and 14 with veterans with SCI&D). Most interviewees had experienced at least one weather-related natural disaster
Veterans with SCI were usually evacuated to unaffected areas or were admitted to SCI centers. Previous disaster experiences provided lessons to guide providers’ and veterans’ actions. Pre-established response plans served as useful starting points. Family and local agencies’ social support was essential for veterans to attain a sense of personal preparedness. The above information was used to develop tools for disaster preparedness.
B. Schmitt(IIR 02-080)
VHA is particularly vulnerable to a postal attack directed at government facilities. Thus, it has an interest in identifying the most advantageous response to small and large-scale bioterrorist events
To conduct a cost-effectiveness analysis comparing response strategies to a small and a large-scale anthrax attack
A decision analytic model was used to compare 3 basic response strategies to a small scale anthrax attack. The optimal response to a mass inhalation anthrax attack was evaluated. Outcomes included costs, Quality-Adjusted Life Years, and incremental cost-effectiveness
For the small-scale anthrax attack, the least costly strategy was administration of antibiotics post-attack; post-attack antibiotic and post-attack vaccination strategy was the most effective. Pre-attack vaccination was the least effective. Pre-attack vaccination was preferable to post-attack antibiotics alone when the probability of anthrax exposure was ≥16%. For the large-scale mass attack scenario, analysis is in progress
Systematic Literature Review
A systematic literature review was conducted to synthesize what is known about VHA emergency management research. Specifically, the review answered the following research questions: 1. What is the role of VHA in emergency management, including mitigation, preparedness, response, and recovery? 2. For each of the identified VHA emergency management activities, what recommendations (“lessons learned”) were made to improve the activity around mitigation, preparedness, response & recovery? 3. What veteran health needs have been identified as important in emergency management? Results of the review are presented elsewhere.6
Achieving Consensus on Research Priorities
The purpose of the VHA Comprehensive Emergency Management Program Evaluation and Research Conference was to bring together researchers and practitioners in a common forum to discuss and make recommendations regarding the direction of future VHA program evaluation and research on emergency management. Participant affiliations included VHA, various universities, CDC, the Department of Defense, NIH, and AHRQ, and other institutions.
After several context-setting presentations about VHA’s role in emergency management, attendees participated in one of five workgroups: Behavioral Health (e.g., mental health; substance use/abuse; psychological first aid; the “worried well”); Workforce (e.g., education/training of personnel; VHA’s Disaster Emergency Medical Personnel System (DEMPS); competing family concerns); Communication and Information Flow (e.g., decision-making; inter-organizational collaboration; risk communication); Sustainability and Resilience (e.g., quality improvement; community resilience); and Systems Capabilities (e.g., broad health systems issues such as evacuation, pandemic influenza; methodological considerations when conducting research in this field; inter-organizational collaboration).
VHA’s Emergency Management Research Agenda
Behavioral Health
The Behavioral Health workgroup (e.g., mental health; substance use/abuse; psychological first aid; the “worried well”) was tasked with identifying and prioritizing VHA emergency management research issues related to the mental health needs of individuals impacted by a disaster or mass casualty event. While the conversation did include some discussion of VHA workforce needs (e.g., training and psychological support) as well as the mental health impacts of disasters on VHA and VHA’s role in providing care for the larger community, most of the workgroup’s discussion focused on preventing and treating post-disaster development or exacerbation of behavioral health problems in the veteran population. Because VHA provides ongoing medical and support services for many veterans with psychological and substance use disorders, addressing the impact of large scale emergencies and disasters on behavioral health needs was considered to be of particular significance to VHA.
Priorities
Key Questions/Research Topics
Workforce
The Workforce workgroup (e.g., education/training of personnel; Disaster Emergency Medical Personnel System (DEMPS)9; competing family concerns) focused on issues regarding: designing and evaluating effective education and training strategies for health care personnel, establishing competency guidelines, effectively engaging health care providers in decision making related to emergencies, DEMPS teams, and how to address employees’ competing concerns for the safety of their own family members. There was a general consensus that a fair amount of funding has been dedicated to training and education, but that rigorous research about the effectiveness of training and education programs is lacking. Furthermore, future effectiveness research should differentiate demonstrating competencies of individuals from system capacity, which is dependent on infrastructure. The workgroup recognized the importance of VHA’s work with various federal partners, and that the manner in which it interacts with other federal agencies is a critical area of research regarding workforce issues.
Priorities
Key Questions/Research Topics
Communication & Information Flow
The Communication and Information Flow workgroup (e.g., decision-making; inter-organizational collaboration; risk communication) focused on a wide array of topics related to emergency management planning issues within VHA, specifically crisis communication, risk communication, communication tools, and community collaboration applicable to the overall healthcare system, veterans, staff, and the community. The group expressed the potential concern that VHA’s organizational culture may be overly driven by protocols and standards, and questioned whether communication could effectively be structured to make and disseminate clinical and strategic decisions to veterans, staff, and local communities in an effective and time-efficient manner given these concerns. The group indicated that it would be valuable to identify triggers that lead to the effective dissemination of information from VHA to the public, and wondered how those mechanisms would be altered by a public health emergency. In this regard, the workgroup noted that VHA could also draw on the expertise of its federal and other partners.
Priorities
Key Questions/Research Topics
Sustainability and Resilience
The Sustainability and Resilience workgroup (e.g., dual-use systems that may improve the quality of care delivered outside of a disaster situation as well as in the event of an emergency; community resilience) met to discuss the sustainability of resources for emergency preparedness and response, and was asked to consider areas in which to invest scarce resources; quality and cost; how to leverage existing systems or to establish “dual-use systems” that provide benefits both under non-emergent and emergent situations; challenges related to the ebb and flow of funding related to the recency and size of a domestic disaster; and the resilience of veterans and VHA, as well as community resilience in general. The workgroup stressed the importance of disaster research funding and recommended that such funding be increased as a prerequisite for a successful emergency management research agenda and its ongoing implementation.
Priorities
Key Questions/Research Topics
Systems Capabilities
The Systems Capabilities workgroup (e.g., broad health systems issues such as evacuation, pandemic influenza; methods; inter-organizational collaboration) discussed the broader healthcare system and population issues applicable to all healthcare systems, although it focused primarily on VHA-specific issues while considering both internal and external concerns. Using both experience with current practices, including a discussion of actual operational decisions made during the response by VHA and others to Hurricane Katrina, as well as an assessment of current gaps in the field’s understanding, this workgroup identified various research priorities. Much of the workgroup’s discussion concerned the potential for VHA to become a leader in developing evidence-based standards for emergency management. The workgroup noted that VHA’s facilities and other resources provide an invaluable “laboratory” to strengthen national emergency management research capabilities. Resources noted by the workgroup included the recognition that VHA facilities that provide care for the most complex inpatient cases are required to have academic resource centers in their facilities. In addition, VHA staff with a military background often have experience either training for or actually having responded to a disaster. Furthermore, VHA currently makes resources available to the local community, including pamphlets that describe how to respond to a local emergency, and plays an extensive role in national emergency response. Finally, in rural areas, VHA may be the sole federal presence in the community and is often relied upon as the primary source of federal distribution, care and support. Members of the workgroup who had been part of the Katrina response also discussed issues surrounding surge capabilities where healthcare workers from neighboring institutions were farmed out to distant facilities because their hospitals were closed.
Priorities
Key Questions/Research Topics
Building an Infrastructure for Fostering the Conduct of VHA Emergency Management Research
Based on the first three steps, the research team recommended a variety of measures to assure that there is adequate infrastructure within VHA to support the implementation of the research agenda. We recommended that a VHA agenda-setting process be reconvened within five years to assess progress on implementing the agenda and to establish new directions for subsequent years. The current research agenda was developed based on the best available data at the time. We anticipate that VHA’s investments in emergency management program evaluation and research will continue to yield rapid advances. This translates into a rapidly changing landscape, and a new set of knowledge and investigators who should be brought together to reappraise, re-energize, and recommit to the next phase of VHA emergency management evaluation and research. Although an updated agenda-setting conference has not been reconvened as of 2016, the initial conference was followed in subsequent years by annual meetings (Advancing and Redefining Communities for Emergency Management) that continue to bring together VA and non-VA researchers, practitioners, and policy-makers to share evidence-based practices and discuss the current state of emergency management research.
Some key differences exist between the VHA and other hospitals and healthcare facilities. For example, VHA has a well-integrated electronic medical system. Private facilities have begun to expand these capabilities in recent years. Electronic medical systems have advantages, but do require power to operate, and thus may require paper backups or other options during some disasters. In addition, VHA has a wide array of facilities that serve various populations, including residential facilities that serve Veterans with substance use disorders and various residential facilities for homeless Veterans.
In addition, it was recommended that efforts be made to increase the visibility of VHA’s emergency management research and its potential to serve as a laboratory for emergency management research for the Nation. Hospital systems often focus on healthcare-related issues at the expense of applying findings from the broader disaster-related literature.22,23,24 It was hoped that issues such as this could be explored within VHA for the benefit of both VHA and the nation. In particular, VHA should maintain and expand a searchable database of published articles and unpublished reports related to VHA emergency management program evaluation and research that would provide support to VHA researchers interested in VHA emergency management research opportunities and collaborations. This effort could lead to the establishment of a multi-component, web-based emergency management evaluation resource clearinghouse that would make emergency management research and evaluation resources more readily available and accessible to researchers and practitioners. Similarly, the establishment of a VHA Comprehensive Emergency Management Program Evaluation Center would enhance VHA’s mitigation, preparedness, response, and recovery activities in the event of emergencies and disasters. The Center’s goal should be to develop an evidence base by which VHA contributes to the development, evaluation and improvement of healthcare services and programs that (1) strengthen VHA’s CEMP, and (2) position VHA as a national leader in emergency preparedness and response. As a result of these recommendations, VHA established the Veterans Emergency Management Evaluation Center (VEMEC) in July 2010. VEMEC continues to this day.
Conclusions
Using a systematic evidence base and consensus development process among stakeholders within and outside VA, we report on the first national VA comprehensive emergency management program evaluation and research agenda. VA provides a unique national laboratory for the conduct of high quality research that will improve VA’s and our Nation’s emergency medical and public health preparedness and the role of health delivery systems in that endeavor. To effectively foster the conduct and expansion of emergency management evaluation and research within VA, the consensus was that VA needs to build program evaluation capacity, increase the awareness and visibility of VA’s emergency management research, and build bridges to research partners at agencies and organizations with longstanding commitments to advancing emergency management research.
Corresponding Author
Aram Dobalian: [email protected]
Competing Interests
The authors have no financial relationships or conflicts of interest to disclose.
Data Availability
All relevant data are available from the figshare repository: https://dx.doi.org/10.6084/m9.figshare.3085807.
Methods: SPEED reports medical consultations based on 21 syndromes covering a range of conditions from three syndrome groups: communicable diseases, injuries, and non-communicable diseases (NCDs). We analyzed consultation rates for 150 days post-disaster by syndrome, syndrome group, time period, and health facility type for adults as well as for children under the age of five.
Results: Communicable diseases had the highest consultation rates followed by similar rates for both injuries and NCDs. While communicable diseases were the predominant syndrome group for children, wounds and hypertension were common syndromes observed in adults. Village health centers had the most consultations amongst health facilities, but also showed the highest variability.
Discussion: Children were more vulnerable to communicable diseases compared to adults. Community health centers showing consistently high consultation rates point out a need for their prioritization. The predominance of primary care conditions requires disaster managers to focus on basic health care and public health measures in community health centers that target the young, elderly and impoverished appropriate to the time period.
]]>Introduction
Typhoon Haiyan was a category five typhoon, which made landfall in the Philippines on November 8, 2013. It made 6 landfalls in the Visayas and Palawan and caused considerable damage to these regions. It affected around 16 million people and killed more than six thousand.1,2 It is considered a sudden onset disaster with prolonged health consequences.1,3
The Health Emergency Management Bureau (HEMB) of the Philippine Department of Health (DOH) activated the Surveillance in Post Extreme Emergencies and Disasters (SPEED) during the response to Typhoon Haiyan. SPEED is a syndromic surveillance system for health facilities that monitors 21 syndromes. Reports can be transmitted manually, via mobile or the Internet. SPEED runs in parallel with the regular epidemiologic reporting system of the DOH. SPEED’s database records consultation rates for 21 syndromes. It enables early detection of communicable diseases, non-communicable diseases, and injuries, monitors syndrome trends, and guides the DOH’s disaster response.4,5
Typhoon Haiyan was a distinct event that disrupted health systems of various regions. Ensuing storm surge caused most of the damage to the population and infrastructure, such as water, electricity, and telecommunication. Typhoon Haiyan dealt a severe blow to the public health system with damages to the tune of 26 million US dollars (USD). The damage to the health infrastructure including 42 hospitals, 95 community health centers and 427 village health centers alone accounted for 19.2 million USD.1,6
Typhoons in general can pose a risk for the outbreak of infectious diseases. Such outbreaks are usually endemic to the affected area and not unfamiliar to the local medical personnel. Expected diseases include watery diarrhea, acute respiratory infections, measles, malaria and dengue. The environmental conditions of overcrowding, increased vector spread, lack of clean drinking water, and hygiene facilities contribute to these conditions.7,8,9,10 Thus humanitarian organizations prioritize these infectious diseases in their disaster response.11
Although the DOH and the World Health Organization (WHO) issued publications on Typhoon Haiyan none of these studies include a detailed account of the disaster’s health impact.1,2,6 In 2015 Martinez et al. analyzed SPEED and conducted focused group discussions to show the health impact of non-communicable diseases during Haiyan.12 In 2016 Salazar et al. used the SPEED database to, analyze the health impact of three disasters from 2013 including Typhoon Haiyan. This analysis, however, did not give detailed information on individual syndromes, health facilities, and children.10 The main objective of this study is to analyze the health impact of communicable diseases, injuries, and non-communicable diseases (NCD) during Typhoon Haiyan using the SPEED database including descriptions of individual syndromes and the use of health facilities by different age groups during disaster response and recovery.
Methods
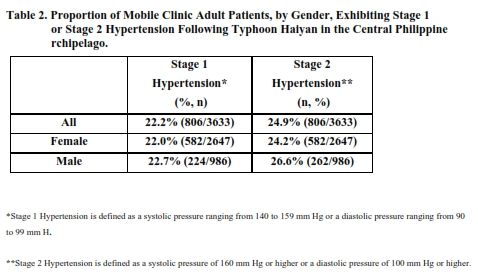
This is a descriptive study of an existing database of the Health Emergency Management Bureau. SPEED uses aggregated data from health facilities in disaster affected areas. This study analyzes SPEED data from health facilities in the Eastern Visayas region, one of the four regions affected by Typhoon Haiyan, from November 8, 2013 to March 28, 2014.6
The database comprises reports that detail the number of consultations per day by health facility for two age groups (<5 vs. ≥5 years of age).4 This study categorizes all syndromes into three groups: communicable diseases, injuries, and NCDs similar to the study by Salazar et al. from 2016.10 Communicable diseases include the following syndromes: acute bloody diarrhea, acute flaccid paralysis, acute hemorrhagic fever, acute jaundice syndrome, acute respiratory infection, acute watery diarrhea, animal bites, conjunctivitis, fever, fever with other symptoms, skin disease, suspected leptospirosis, suspected measles, suspected meningitis, and tetanus. Fractures and wounds, including bruises and burns are considered syndromes for injuries. The following are syndromes for NCD’s: acute asthmatic attack, acute malnutrition, high blood pressure, and known diabetes mellitus.4,10
To calculate consultation rates per day according to health facility, age group as well as all ages combined, we divided the respective number of consultations by the corresponding population of the catchment area of each health facility. The catchment area was estimated according to the type of health facility i.e. village health centers, community health centers, hospitals, evacuation centers, mobile clinics, foreign medical team clinics, and foreign medical team hospitals. For village health centers and evacuation centers the village population was defined as the catchment area. For community health centers and hospitals the municipality or city population was used. Less observed health facility types (mobile clinics 1%, foreign medical team clinics 2%, and foreign medical team hospitals 0.4%) were merged with the best fitting group as follows: mobile clinics and foreign medical team clinics with village health centers and foreign medical team hospitals with hospitals. The population data used is based on the 2010 census from the Philippine Statistics Office.13,14
Mean consultation rates per day with 95% confidence intervals and t-tests comparing age groups and time periods were calculated using Stata Version 13.15,16 Scatter plots and splines were used to visualize the trend in syndrome morbidity. Splines are based on regressions, joining points to fit a particular shape.17 Consultation rates were presented per 10,000 individuals per day as this number is routinely used in the literature for emergency health kits.10,18 Additionally, rates within two months (≤60 days) were compared to rates after two months (>60 days) as this was identified to separate response and recovery.10
As this is a descriptive study of an existing database using aggregated data, the Institutional Review Board of Heidelberg University deemed the study exempt from full review. Prior to the start of the study, the SPEED database for Typhoon Haiyan was requested from the director of HEMB. HEMB did an initial validation of the Haiyan data.10 All SPEED database reports were handled with confidentiality by the authors of this study. SPEED consists of aggregated data from health facilities, which does not include individual patient information, thus also ensuring the confidential and anonymous nature of the database.
Results
As part of disaster disease surveillance conducted by HEMB and DOH, there were 3,425 SPEED reports for Typhoon Haiyan in the Eastern Visayas region within 150 days post-disaster. For mean rates, communicable diseases had overall the highest rates, 47.3 per 10,000 individuals, followed by similar rates for both injuries (5.9) and NCDs (6.0). Looking at consultation rates over time, the representative syndromes for communicable diseases, injuries, and NCDs are acute respiratory infections, wounds, and high blood pressure respectively. These syndromes were selected because they had the highest rates among all syndrome groups (see Table 1). The spline and scatter plot shows a peak in consultation rates around day 20 to 25 for all three syndromes. Thereafter, rates decrease and stabilize around day 50 post-disaster. Acute respiratory infections showed a much more prominent increase in consultation rates compared to wounds and high blood pressure (see Figure 1).
Table 1: Syndrome rates per 10,000 individuals separated by time post-disaster and by age
Syndrome
Total
≤ 2 months
> 2 months
Difference between ≤ 2 months and > 2 months
< 5 years of age
≥ 5 years of age
Difference between < 5 years and ≥ 5 years
Communicable diseases
Acute respiratory infection
36.0
64.0
11.1
52.9 (p<0.01)
112.4
25.6
86.9 (p<0.01)
Skin disease
4.5
8.2
1.2
7.0 (p<0.01)
13.8
3.2
10.5 (p<0.01)
Acute watery diarrhea
2.5
4.6
0.6
4.0 (p<0.01)
11.4
1.3
10.0 (p<0.01)
Fever
2.3
4.1
0.7
3.4 (p<0.01)
8.4
1.4
6.9 (p<0.01)
Fever with other symptoms
0.8
1.3
0.3
1.0 (p<0.01)
1.4
0.7
0.7 (p=0.06)
Animal bites
0.5
0.8
0.2
0.6 (p=0.03)
1.1
0.4
0.8 (p=0.11)
Conjunctivitis
0.3
0.5
0.1
0.4 (p<0.01)
0.5
0.3
0.2 (p=0.19)
Suspected leptospirosis
0.1
0.3
<0.1
0.3 (p=0.01)
0.2
0.1
0.1 (p=0.52)
Acute bloody diarrhea
0.1
0.2
<0.1
0.2 (p<0.01)
0.3
0.1
0.3 (p=0.01)
Suspected meningitis
0.1
0.2
<0.1
0.2 (p=0.24)
0.1
0.1
<0.1 (p=0.78)
Suspected measles
0.1
0.1
0.1
<0.1 (p=0.47)
0.5
<0.1
0.4 (p=0.07)
Acute hemorrhagic fever
<0.1
<0.1
<0.1
<0.1 (p=0.34)
0.1
<0.1
<0.1 (p=0.28)
Acute jaundice syndrome
<0.1
<0.1
<0.1
<0.1 (p=0.04)
<0.1
<0.1
<0.1 (p=0.03)
Tetanus
<0.1
<0.1
<0.1
<0.1 (p=0.12)
<0.1
<0.1
<0.1 (p=0.18)
Acute flaccid paralysis
<0.1
<0.1
<0.1
<0.1 (p=0.02)
<0.1
<0.1
<0.1 (p=0.03)
Communicable disease total
47.3
84.5
14.2
70.3 (p<0.01)
150.2
33.3
116.9 (p<0.01)
Injuries
Open wounds & bruises/burns
5.8
10.7
1.4
9.3 (p<0.01)
6.2
5.7
0.4 (p=0.74)
Fractures
0.1
0.2
<0.1
0.2 (p=0.01)
0.3
0.1
0.2 (p=0.25)
Injury total
5.9
10.9
1.4
9.5 (p<0.01)
6.4
5.8
0.6 (p=0.65)
Non-communicable diseases
High blood pressure
4.7
8.0
1.8
6.2 (p<0.01)
0.1
5.4
5.3 (p<0.01)
Acute asthmatic attack
0.9
1.6
0.3
1.3 (p<0.01)
2.0
0.8
1.2 (p<0.01)
Known diabetes mellitus
0.4
0.7
0.1
0.6 (p<0.01)
<0.1
0.4
0.4 (p<0.01)
Acute malnutrition
<0.1
0.1
<0.1
0.1 (p=0.04)
0.2
<0.1
0.2 (p=0.22)
NCD Total
6.0
10.3
2.3
8.1 (p<0.01)
2.2
6.6
4.3 (p<0.01)
Fig. 1: Consultation rates per 10,000 individuals for acute respiratory infections, wounds, and hypertension.
A similar number of reports was observed within two months (n=1,614) and after two months (n=1,811) post-disaster. Within two months post-disaster, acute respiratory infections also accounted for the highest consultation rates with 64.0 per 10,000 individuals. Wounds and hypertension had consultation rates of 10.7 and 8.0 per 10,000 individuals respectively. After two months post-disaster the rates for all three syndromes were significantly lower: acute respiratory infections (11.1), wounds (1.4), and hypertension (1.8).
Rates for the whole 150-day period decreased in the following order: acute respiratory infections, open wounds, high blood pressure, skin disease, acute watery diarrhea, and fever. Within two months post-disaster, eight syndromes showed consultation rates higher than 1 per 10,000 individuals compared to six for the whole period. The additional two syndromes were acute asthmatic attack and fever with other symptoms. After two months post-disaster, only four syndromes were above 1 consultation per 10,000 individuals per day. These were acute respiratory infections, open wounds, high blood pressure, and skin disease. Comparing consultation rates for these two periods all syndromes show higher consultation rates in the first two months post-disaster. Only four syndromes displayed differences with p values greater than 0.05; these were meningitis, suspected measles, acute hemorrhagic fever, and tetanus. The top eight syndromes: acute respiratory infections, open wounds, hypertension, skin disease, watery diarrhea, fever, asthma, and fever with other symptoms showed differences greater than 1 consultation per 10,000 individuals and p values less than 0.01 (see Table 1).
The top eight syndromes showed differences when analyzed according to age group. Acute respiratory infections, skin disease, acute watery diarrhea, and fever showed the highest consultation rates for children under the age of five. Acute respiratory infections had the highest consultation rates for adults followed by wounds, hypertension, and skin disease. Communicable diseases had significantly higher rates in under-five-year old children specifically for acute respiratory infections, skin disease, acute watery diarrhea, and fever. Injuries had similar rates for both age groups. While NCDs in form of hypertension and diabetes were more common for adults, asthma was more common for children under the age of five (see Table 1).
When grouped according to health facility type, most records in SPEED were contributed by community health centers and hospitals with 54% and 30% respectively. Village health centers had the highest consultation rates among the four health facility types and also had the highest variability across time seen in its 95% confidence interval and difference in the mean rates (see Table 2).
Table 2: Consultations per 10,000 individuals per day per health facility
Health Facility Type
# of SPEED reports
Mean with 95% confidence interval
Community Health Center
1850
25.0 (20.3-29.7)
Evacuation Center
39
19.5 (0-43.9)
Hospital
1039
7.0 (6.5-7.6)
Village Health Center
497
299.0 (247.1-350.9)
Discussion
This study provides a detailed analysis of the conditions seen in health facilities in the aftermath of Typhoon Haiyan. It illustrates that communicable diseases were the most common syndrome group, and that acute respiratory infection was the most common of the 21 syndromes. Under-five-year old children displayed higher rates for communicable diseases, similar rates for injuries, and lower rates for NCDs in comparison with adults. The highest consultation rates recorded came from village health centers followed by community health centers.
Syndromes which were consistent in their consultation rates throughout the whole period, such as meningitis, suspected measles, acute hemorrhagic fever, and tetanus all require referral to tertiary care.19 These syndromes showed rates of less than 0.1 for the whole 150-day post-disaster period, indicating nevertheless a potential risk these syndromes pose during response and recovery periods. The most common syndromes recorded in the SPEED database represented primary care conditions. According to Connelly et al. in 2004, acute respiratory infections and diarrhea, syndromes which were also observed in this study, account for the majority of morbidities in emergencies. Acute respiratory infections and diarrhea are attributed to over-crowding in shelters and lack of quality water services respectively.20
Communicable diseases were more prominent in children under five manifesting as acute respiratory infections, skin disease, acute water diarrhea, and fever. A study concluded in the aftermath of Hurricane Katrina in the United States in 2005, showed that pediatric consultations included respiratory conditions, skin ailments, and under-nutrition. Respiratory conditions reported were acute respiratory infections and allergic rhinitis while skin conditions included bacterial and fungal infections.21 Furthermore, a systematic review from 2013 showed that the most common pediatric themes found in the literature for emergencies and disasters included infectious conditions, vaccine-treatable diseases, hygiene-related ailments, and wounds.22
As expected NCDs were more visible in adults; hypertension had the third highest rate. Moreover, hypertension and diabetes displayed a significant difference in rates within and after two months post-disaster. Another study on Hurricane Katrina found that 40% of those seeking consultations came because of chronic conditions such as hypertension. 20% came in order to get medication for pre-existing chronic conditions.23 This may be due to an increase in demand for chronic disease treatment because of health system disruption.24 In the case of Typhoon Haiyan, first-line health providers saw that patients with NCDs experienced a lack of supply of medications and basic necessities such as food and clothing.12 The need for basic provisions for survival may have pushed these patients to seek consult for pre-existing conditions thus causing an increase in the consultation rates within the first two months post-disaster.
Haiyan’s mortality profile and magnitude causing disaster response delay contributed to the conditions observed in SPEED. Most storm surge mortalities are due to drowning.25 This is also true for Typhoon Haiyan. In a case control study after the typhoon, which looked into the risk factors associated to mortality, the deaths observed were all due to drowning.26 Since the disaster had a high death toll (6,300 people were killed),1 consultation rates for fractures were low. Open wounds, the more benign syndrome, had the second highest syndrome rate. Moreover, the initial responders were also victims since their health facilities and homes had been destroyed by the typhoon. It took the local responders from neighboring regions two days before they reached the hardest hit areas.1 Furthermore, foreign medical teams needed a minimum of three days after arriving in the country to be operational. The peak of functional number of foreign medical teams was only achieved 22 days post-disaster.3 The delay in the response to Typhoon Haiyan may have shifted the profile of the diseases seen in SPEED to more primary care conditions.
The top syndromes highlighted in this study can be addressed with proper diagnosis, appropriate medications, and wound cleaning & dressing.19 Due to their permanent vulnerability, poor populations and people with chronic conditions should be considered for targeted interventions during response and recovery phases of disasters.24 In general, communicable diseases, injuries, and NCDs can be addressed by providing continuous basic health services, water, sanitation and hygiene, nutrition, public health surveillance, disease control, and proper shelter to vulnerable groups namely poor, young, and elderly patients.10,11,20,27
For most syndromes regardless of need for referral, rates within two months were significantly higher than those after two months. In the case of Typhoon Haiyan, the Interagency Standing Committee downgraded its emergency response level 93 days or three months post-disaster. This was in contrast to the national government decision to move from disaster relief to recovery seven months post-disaster.28 Compared to these bureaucratic decisions by both national and international agencies, SPEED provides an evidence-based junction between disaster response and recovery seen in the trends of consultations post-disaster. The sustained decrease in consultations around day 50 can be constituted as the demarcation between disaster response and recovery based on disease surveillance trends.10
We additionally calculated median values to take into account outliers in the data set, but interpretation of the results remained similar to mean rates. Due to the lower number of SPEED reports for evacuation centers and village health centers the mean rates had wider confidence intervals compared to community health centers and hospitals. This high variability prompts further research in health facility utilization during disasters.
Typhoon Haiyan was a mega-disaster with extensive disruption of the health system. The Eastern Visayas region had 22 hospitals, 53 community health centers, and 113 village health centers damaged comprising 52%, 56%, and 26% respectively of each of the damaged health facility types across all four regions.2 Since SPEED received most data from community health centers and hospitals we suppose that these health facility types were the ones to be still operational. Another explanation might be that disaster managers and health ministry officials prioritized these central health facilities as the main reporting centers due to limited capability of logistics and transportation to get to the village health centers further away. This prioritization of community health centers and hospitals was reflected in the publications of the WHO Philippine Country Office and the DOH on community health centers and hospitals affected by Typhoon Haiyan. Community health centers were described as the focal point of primary health care. The local health executives govern the management of village health centers in their catchment areas through community health centers. Moreover, these act as feeders to nearby hospitals for tertiary care.2,6
This study demonstrates the use of SPEED for planning response and recovery activities. In the prioritization of health facilities to be reconstructed or rehabilitated, we propose that the health facilities showing significantly higher rates of consultations, namely community health centers, should be prioritized immediately. Logistics for required medications and supplies for different age groups should be planned according to their percentage in the local population. Planning for medicines, supplies, and equipment as well as training on protocols for prominent diseases of children and aging populations should be emphasized. These populations are also less mobile thus access to health services, both financial and geographic, should be considered. As children and elderly are more vulnerable to environmental factors such as cold and wet weather,29 priority should be placed on shelter for these populations.
The rates for Typhoon Haiyan should be the benchmark for future planning purposes. Typhoon Haiyan was a category five typhoon and the strongest typhoon ever recorded in Philippine history.2 Thus, for now, it is the best template for preparing for the worst possible scenario.
Being a syndromic surveillance system, SPEED has some inherent limitations with regard to the generalizability of the results of this study. The findings of the study refer to health facility data in the Eastern Visayas region and cannot be interpreted as being representative of the whole population affected. Moreover, the population data used to calculate the consultation rates did not take into account the actual population immediately before or after Typhoon Haiyan. Out-migration from the affected areas has not been taken into account either. With regard to SPEED itself, it has to be noted that in some of the affected areas, the system was not operational until one week post-disaster.5 As the syndromes are not that specific and health facilities were not able to report daily, the results should be read as rough estimates rather than exact values. Thus disaster managers still should also consider their extensive experience and integrate it with the findings of our study.
Conclusions
The predominance of primary care conditions seen in the study may be used for planning for future disasters and signals disaster managers to focus on basic health care and public health measures. The trends observed for consultation rates across time may be used as guides for disaster response and recovery. Interventions targeting young, elderly, and impoverished populations are recommended. Community health centers should be prioritized in recovery and rehabilitation efforts.
Competing Interests
The authors have declared that no competing interests exist.
Corresponding Author
Miguel Antonio Salazar: [email protected]
Ethics
This study uses the 2013 data from Surveillance in Post Extreme Emergencies and Disasters (SPEED), an existing database using aggregated health facility data of the Health Emergency Management Bureau of the Philippine Department of Health. The authors of the study received the SPEED reports as aggregated data and did not have access to individual patient information.
Data Availability
The data from this study are owned by the Health Emergency Management Bureau of the Department of Health of the Republic of the Philippines. As these are government-owned data, their release is subject to the approval of the Director of the Health Emergency Management Bureau. Requests for this data set may be sent to Director Gloria J. Balboa, MD, MPH, MHA of the Health Emergency Management Bureau via [email protected], or through the following address: Health Emergency Management Bureau, Department of Health, San Lazaro Compound, Tayuman, Sta. Cruz, Manila, 1003 Philippines.
Authors’ Contribution
The authors of this manuscript were involved in the conception and design of the study or have contributed to the acquisition, analysis, or interpretation of the data of the study. They were part in its critical revision. They have agreed to be accountable for all aspects of the work.
MAS wrote the manuscript, conceptualized the study, interpreted the results, and collated the responses and comments from other authors. AP took part in the conception of the study and analyzing the results. RL was vital in acquiring data and analyzing the results. AP and RL contributed to the revision of the manuscript. VW contributed to the writing of the manuscript, the conceptualization of the study and the analysis of the results.
Commentary
As physicians, we are reminded of Sir William Osler’s 1906 speech to graduating medical students when he asserted that: “Medicine is the only world-wide profession, following everywhere the same methods, actuated by the same ambitions, and pursuing the same end. This homogeneity, its most characteristic feature, is not shared by the law or religion”, nor the “extraordinary solidarity which makes the physician at home in any country.”1
In the century that followed, no other profession has exhibited the influential number of international associations, societies and collaborative efforts as has medicine. The end of the Cold War brought multiple humanitarian crises and the development of international academic and educational training programs designed to prepare humanitarian workers for these complex global tasks. The rigorous curriculum includes the unique roles and responsibilities that healthcare providers have under the Post-World War II Geneva Convention (GC) and International Humanitarian Law (IHL) which ensures their right to international health neutrality.
Historically, war has caused the loss of countless lives and has ravaged the most vulnerable populations, especially women, children, the elderly and disabled. The humanitarian crises that wars create, and the manner in which the world responds, have changed with every generation.2 Present-day healthcare workers in public hospitals and non-governmental organizations in conflict zones have never faced greater risks. In fact, deaths among all humanitarian workers have outnumbered those of UN Peacekeepers in recent years.3
The cross-border territorial wars that dominated the 20th Century have been replaced by endless religious, ethnic and tribal conflicts that produce neither winners nor losers. The war in Afghanistan has raged on since 1979, in Somalia since 1991, and the recent Yemeni civil war since 2015. Yet, there is something especially abhorrent about the current war in Syria that should gain the attention of every healthcare provider and health policy maker. These alarming statistics are reminders of the egregiously barbaric quest of ancient wars, designed to ensure that no survivor would remain to take revenge:
As of June 2016, 757 healthcare personnel have been killed and 382 premeditated attacks have occurred on 269 separate medical facilities across Syria. One-hundred and twenty-two hospitals have been targeted multiple times.4 In the midst of this misery one cannot forget the US targeted aerial bombing of Médecins Sans Frontières hospital in Kunduz Afghanistan in October 2015 that killed 42 people, including 14 MSF staff members, and wounded dozens more.5
We must take notice and stand in solidarity with our healthcare colleagues in Syria where patients, healthcare workers, and hospitals are under constant threat and attack. We have the obligation to ensure that every health care provider, both civilian and military, on either side of the current conflict in Syria, be made aware of the inherent protections provided them under IHL, including the four GCs of 1949, as well as the principles and rules of IHL applicable to the conduct of hostilities, which include the targeting of hospitals and medical facilities. These principles and rules must be upheld.
Healthcare providers of the militaries involved on both sides of the conflict are granted provisions and protections under international laws clearly referenced in The Hague Statement on Respect for Humanitarian Principles (1991), UN Security Council Resolution 2286 on attacks against medical workers (2016) and military manuals of many States. As an example, the Russian Federation’s Military Manual (1990) states that attack against medical personnel constitute a prohibited method of warfare. The Russian Federation’s Regulations on the Application of IHL (2001) states: “Persons protected by international humanitarian law include medical and religious personnel. Attacks against such persons are prohibited.”
As such, healthcare providers, both civilian and military, including the Assad Government and the Russian Federation, must equally recognize that under IHL, their own medical military personnel, activities, units, transports, and hospitals are guaranteed protection against direct attack themselves (see rules 25 to 30 of the ICRC’s customary IHL study, as well as protections in the Geneva Conventions and their Additional Protocols). IHL requires Parties to ensure respect for IHL, including under common Article 1 to the four GCs. Failure to do so leads to risks of moral, ethical and legal consequences as well as penalties for their actions and inactions.
The World Medical Association (WMA) Regulations in Times of Armed Conflict and Other Situations of Violence6 assert that under IHL, healthcare providers can neither commit nor assist violations of IHL, nor take part in any act of hostility; must advocate and provide effective and impartial care to the wounded and sick (without reference to any ground of unfair discrimination, including whether they are the “enemy”); must remind their authorities of their obligation to search for the wounded and sick and to ensure access to health care without unfair discrimination; must not allow any inhuman or degrading treatment of which physicians are aware; must report to a commander or to other appropriate authorities if health care needs are not met; and must give consideration to how health care personnel might shorten or mitigate the effects of the violence in question, for example by reacting to violations of international humanitarian law or human rights law.
WMA summarizes the ethical obligations of physicians as follows:6
During times of armed conflict and other situations of violence, standard ethical norms apply, not only in regard to treatment but also to all other interventions. The medical duty to treat people with humanity and respect applies to all patients. Governments, armed forces and others in positions of power should comply with the GC to ensure that physicians and other health care professionals can provide care to everyone in need in situations of armed conflict and other situations of violence. This obligation includes a requirement to protect health care personnel and facilities. Privileges and facilities afforded to physicians and other health care professionals in times of armed conflict and other situations of violence must never be used other than for health care purposes.
Physicians should recognize the special vulnerability of some groups, including women and children. Provision of such care should not be impeded or regarded as any kind of offence, nor must they ever prosecuted or punished for complying with any of their ethical obligations. Physicians have a duty to press governments and other authorities to ensure they are planning for the protection of the public health infrastructure and for any necessary repair in the immediate post-conflict period. Necessary assistance, including unimpeded passage and complete professional independence, must be granted.
Healthcare Parties must be Identified and protected by internationally recognized symbols such as the Red Cross, Red Crescent or Red Crystal. Hospitals and health care facilities situated in areas where there is either armed conflict or other situations of violence must be respected by all combatants. Physicians must be aware that, during armed conflict or other situations of violence, health care becomes increasingly susceptible to unscrupulous practice and the distribution of poor quality / counterfeit materials and medicines, and must attempt to take action on such practices. As such, the WMA supports the collection and dissemination of data related to assaults on physicians, other health care personnel and medical facilities, by an international body. Assaults against medical personnel must be investigated and those responsible must be brought to justice.
In Syria, Yemen, and Afghanistan as well as in many other nations in conflict around the world, the following remedies must be implemented immediately:
1. The establishment of healthcare safe zones in conflict regions to ensure the integrity of hospitals, clinics, and medical centers.
2. Allowing safe and unfettered passage of medical supplies, equipment, and personnel.
3. Cessation of all attacks on patients, pre-hospital personnel, and hospital medical staff.
4. Recognition by all parties of the neutrality of health care workers and their rights and responsibilities to care for any sick and injured patient, regardless of their nationality, race, religion, or political point of view.
The authors are representatives of academic training centers worldwide that provide global health professionals with education and training in humanitarian assistance where every healthcare provider, both civilian and military, is made aware of the inherent protections accorded to them under international law.7 In the same Oslerian spirit of over a century past, we condemn absolutely these deplorable actions in Syria and demand their immediate cessation; and we ask healthcare providers globally to do the same.
Competing Interests
The opinions expressed in this article are the authors’s own and do not reflect the view of their affiliated institutions.
Corresponding Author
Frederick M. Burkle, Jr.: [email protected]
Methods: To achieve this goal, it was undertaken: i) qualitative evaluation to assess the impact of earthquake on services and facilities of the university, the emergency preparedness and the measures adopted to face the emergency, ii) survey on the role played by Student Associations, both in emergency preparedness and response, according to students’ perception; iii) quantitative analysis to measure changes in the enrollment trend after the earthquake, and how university policies could curb students’ migration.
Results: The policies adopted by the University allowed to diminish students’ migration; however, the measures taken by the university were based on an ad hoc plan as no emergency and continuity plans were prepared in advance. Similarly Student Associations got involved more in restoration activities than in emergency preparedness and risk awareness promotion.
Discussion: Greater awareness and involvement are essential at each level (administrators, faculties, students) to plan in advance for an adverse scenario and to make important steps forward in understanding and embracing a culture of safety. The present paper is starting point for future research to deepen the emergency preparedness of Universities and the role that Student Associations may play to support and spread such a culture of safety.
]]>Introduction
At 3:32 a.m. (UTC+1) on 6 April 2009 an earthquake of Mw=6.3 hit the historical downtown of L’Aquila and its hinterland. The mainshock was anticipated by a long lasting seismic cluster (Ml<4.0) that begun in the second half of December 2008. Luckily, two major shakes of Ml=3.9 and Ml=3.5 developed few hours before the April 6th mainshock, alerted the population and induced part of them to flee the buildings and spend the night outside 1,2. The earthquake caused 308 dead, 1500 injured and 63000 displaced. Among the dead, 55 were university students, of which 8 died in the collapse of a university dormitory. Had the earthquake occurred in daytime, the people involved in the collapse of ancient public buildings would have been probably much higher. The high seismic risk in Italy depends not only on the frequency and the intensity of the earthquake hazard, but also on the vulnerability of the built environment. The Italian territory is dotted by many ancient buildings liable to collapse during earthquake 1,2,3,4,5,6. The government agency responsible for promotion and coordination of disaster risk reduction activities in Italy is the Department of Civil Protection (DPC), which was established by Law 225/92, recently amended by Law 100/2012. Other and more specific framework laws (e.g. L.D. 81/2008 8, M.D.10 March 1998 7) define the responsibilities and duties of certain public agencies, including the universities, in terms of emergency planning and risk reduction. In the specific case of public universities, the Law gives to their government bodies (e.g. the chancellor, the academic senate, and the board of directors) a certain degree of autonomy to decide strategies for disaster risk reduction, including the staffing and organization of an internal emergency management group. Indeed, emergency planning beside improving safety and security of students, is a moral obligation of universities, which also safeguards the execution of their institutional scope, namely higher education and professional training activities. The inability to provide basic services like courses, exams, graduation, research, after a disaster, may fatally impact a university reputation and financial status. This becomes particularly important, when the university plays a key role in the economy of the local community. At the time of the earthquake, the University of L’Aquila had 23000 students enrolled across its various graduate and undergraduate degree programs; the student population was almost one third of the total number of residents of L’Aquila 9. Hence, the university was a major source of employment and income for the city and its surroundings, as well as a fundamental drive for cultural and social activities of the city. The negative effects endured by the university bore direct consequences on the city, the inhabitants and particularly the students. In this scenario, the students are not just patrons of the university, but also part of the social fabric of the city; thus, students should be involved in the emergency planning processes of both the city and the university. Such involvement happened only in minimal part in the 2009 earthquake. In Italy, as in many other parts of the World, students take part of the university governance process through the Student Associations. These organizations are directly managed by the students and are dedicated to improve all the aspects of students’ life in higher education. Their scope ranges from safeguarding students’ rights (e.g. welfare and representation) to promote social, political and cultural initiatives. Concurrently, Student Associations are an important interface between the university and the local community, contributing to the civic debates and processes 10,11. The University of L’Aquila was not an exception to this, and four major student organizations were active at the time of the earthquake: the “Azione Universitaria” (rightist political view), “Lista Aperta” (catholic oriented), “Unione degli Universitari” (leftist political view), and “Modus” (non-partisan). All the Srudent Assoctions took part to the University politics with initiatives on the “right to education” and student safety and security. Analyzing the impact of the April 6th 2009 earthquake on the University of L’Aquila both in terms of facilities and business continuity, this study assesses the emergency reparedness and response capability of such university, and the strategies adopted to restore the education activities and avoid students migration to other universities. In addition, emphasis is placed on the role played by Student Associations during pre and post-disaster phases, as well as how the student population perceived the activities performed by these associations.
Emergency management in universities
Over the past years various disasters affected universities and higher education institutions worldwide. For example, Hurricane Katrina’s impacted Tulane and Louisiana State Universities (August 2005). The Midwest seismic event (April 2008). Those events determined economic losses to universities both in terms of structural damages and disruption of academic activities. Indeed, comprehensive pre-disaster planning and preparation can considerably reduce the negative effect of extreme events 12. The US Federal Emergency Management Agency (FEMA) has financed the Disaster Resistant University (DRU) program, in order to develop planning strategies for vulnerability reduction in american universities 13,14. In Canada, universities are not held directly responsible for emergency management; emergency planning and management is coordinate with local authorities 15. In England, Easthope and Eyre 16 published a manual entitled “Planning for and Managing Emergencies: A Good Practice Guide for Higher Education Institutions (HEIs). The authors made a distinction between the emergency planning and the business continuity management. Special attention is dedicated to training, drills and exercises, and emergency communications, with the latter having a key role in the planning processes 16,17. In Italy, the issue of safety and security in Universities was tackled in 2007 by the Italian Universities Chancellors’ Permanent Conference (CRUI), which commissioned a thorough investigation of how emergency management regulations are applied within the public university precincts. The study showed that a vast majority of the Italian universities has developed, within their organizational structure, a Health and Safety Office (HSO) to which are delegated emergency management responsibilities. However, CRUI found that 47.2 % of the universities do not perform emergency planning activities systematically. Therefore, even if the Italian universities started to incorporate safety and security strategies in its official procedures, many steps forward have to be done to turn theory into practice 18. Some hindrances also arise from the Italian law framework on emergency management for universities, which is strictly connected with workplace health and safety 7,8 and it is only focused on the immediate response to minor operational incident (in contained areas or within a classroom or laboratory). The March 10th 1998 Decree of the Italian Ministry of Interiors defines the criteria about the fire control and workplace accident management, drafting evacuation and the fire brigades alarm procedures. As a consequence, disaster prevention or business continuity management is not really contemplated in Italian university, and there is a widespread underestimation of risks by the local emergency managers 18.
University Student Associations and emergency preparedness: a neglected nexus
In spite of the different forms of configuration, management, financing and scope of Student Associations in different parts of the World, a common purpose of these organizations is representing students’ prerogatives to enhance their studying experience (e.g. asking for better school services, curriculum or educational funding). Many Student Associations are nonpartisan, yet such organizations are catalysts of students’ activism and have greatly influenced political debates on both local and global issues. For example, in the United States, France, United Kingdom, and many other countries, the political vehemence of Student Associations reached a high in the 1960s and 1970s during the protests and strikes to end the war in Vietnam and against the invasion of Cambodia 19,20. In the 1980s new subject matters, such as equal opportunities, feminism, environmentalism and humanitarianism, softened the political activism of Student Associations, yielding attention to more local issues of tuition fees or student representation in college governance 21. In Italy most Student Associations have a declared and deep-seated political characterization, and are organized into bodies with a hierarchical structure emulating the country’s political administrative layout. Although the first appearance of organized associations of university students in Italy can be dated back to the 1920, during the Fascist era, it was only after World War II that these associations became truly representative of the whole national students’ community. Indeed, the contestation years of the 1960s and 1970s produced protests and riots activities in Italy too. The ensuing social and civil developments of Italy, weakened the militant components of Italian Student Associations, which by the early 1990s were completely engaged in nonviolent debates. Nowadays, these associations confederated in lists coalescing into three major political views; conservative, catholic-moderate, and liberal-progressive. All these associations operate at the local level electing the “Student Council” which has propositional functions at the Faculty Council, Academic Senate and the University’s Boards of Directors. They also partake into the “National Council of University Students,” a permanent panel which select representative to the “National University Council” (the advisory board of the ministry of education that composed by university’s rectors, faculties, students and employees). Beside these nationwide and chartered Student Associations there exist other, more independent and goal oriented, student organizations. Their scope and inspiring foci can be very different one another, ranging from specific cultural interests, to international student exchange programs, including volunteer services. Unquestionably, Student Associations, in spite of their scope, national vs. local, or their objectives, partisan vs. nonpartisan, are an invaluable resource for the university on a variety of purposes, including students’ safety and security. Yet, this resource is most often completely untapped in terms of disaster prevention and preparedness activities, especially for increasing risk awareness and knowledge transfer. This appear to be true in Italy as well as in many other countries; as a matter of fact, no consistent information about a systematic engagement of Student Associations in disaster risk reduction was found. The potential for this nexus is remarkable, both for developing a culture of safety with younger generations, and for boosting universities’ emergency planning and procedures. Involving students in the campus’ safety and security programs, would increase their awareness of potential hazards and risks in their locale, and train them with protective behaviors and emergency procedures. Gaining students’ attention on such initiatives should not be too challenging, considering the high number of enrollment of students (especially undergraduates) in hazards and disasters related degree programs and courses 22.
Student Associations in L’Aquila
Few days after the earthquake, the National Council of Italian Students (Student Council) unanimously adopted a motion to ask the National Government for prompting the reconstruction of the University of L’Aquila and the restoration of its services. More specifically, the National Council asked the Government to rebuild an high-tech campus with first-class antiseismic standard and to exempt the students from University fees. The Council also led an initiative, named UNILIBER, to gather academic books for the University of L’Aquila in collaboration with the National Civil Protection, Rai-Radio TRE (program Fahrenheit) and the L’Aquila section of the National Youth Corp of Scouts (CNGEI). Since the days after the main shock, the democratic left wing list named “Union of University Students” (U.D.U), which had just gained the majority of seats in any representative local board at the University of L’Aquila, set up an headquarter office inside a container situated in a temporary tents camp close to the College of Natural Science in the village of Coppito. The U.D.U. kept offering logistic assistance to the students residing in the tents camp during the whole emergency. Another volunteer Student Associations named LARES, from the University of Perugia (Central Italy), joined U.D.U. to help managing students’ accommodations in the tent camps of Coppito, coordinating also an information front desk inside the college of Sciences.
Case study
The University of L’Aquila was founded in 1952, and became a full-fledged Italian State University in 1982 academic year. The University is composed of 9 Colleges (Biotechnologies, Economics, Engineering, Humanities, Medicine and Surgery, Psychology, Mathematical Physical and Natural Science, Education Science, Sport Science), 18 Departments and 2 Centre of excellence for research. At the time of the earthquake, the University had 3 campuses within the municipality of L’Aquila (Centro, Coppito, Roio), and others campuses in the neighboring municipalities (Sulmona, Avezzano and Celano). For teh academic year 2008/09, the University offered a broad choice of degree programs and courses: 41 bachelor degrees, 43 Master degrees, 24 Ph.D., 40 specialization schools. The faculty body was composed of 665 persons. During the 2007/08 academid year, on a total of 72000 people living in L’Aquila, 27168 were students. Of these students 37% came from L’Aquila and province; 32% from others Italian provinces; 28% from others provinces of Abruzzo Region; and 3% from abroad (University of L’Aquila Statistics Observatory). According to the Italian Universities templates for governance 32, the University of L’Aquila is an institution with legal personality and teaching, scientific, organizational, financial and accounting autonomy. The government bodies for guidance and control are: the Rector, the Academic Senate and the Boards of Directors 23. The Rector, the legal representative of the University, promotes and coordinates the strategies expressed by the Academic Senate and the Boards of Directors. The Academic Senate performs procedures, planning, coordination and monitoring of teaching and research activities. The Board of Directors manages and controls the administrative, financial and patrimonial activities of the University. In order to reach its institutional goals, the University fields specific facilities: Colleges, Departments and service centers. The Colleges support and manage the education; the Departments coordinate and manage the research activities; the service centers have general competences. The education services and the research activities of the L’Aquila University are almost entirely dependent on State funding (more than 80%). Others funding sources are students’ fees (about 15%) and self-financing obatined by selling services to the private and public sector. Also relevant is the participation of the Student Associations in the government bodies.
Research questions
As discussed in the previous chapters, the Italian universities lack specific regulations on disasters recovery and business continuity mostly because the law framework is limited to standard procedures for minor incidents and emergency management in the workplace. In addition, the tendency to underestimate the risk induces universities to neglect emergency planning activities and drills. The L’Aquila earthquake represented am unusual case study as it struck an area tightly bonded with socio-cultural activities and incomes generated by the university. Furthermore, none of the seven largest earthquakes which hit the Italian peninsula in the last 50 years occurred as close to a major university campus as the one that struck L’Aquila. These circumstances led to the following questions:
RQ1: How did the earthquake affect the University services and facilities?
RQ2: How was the University prepared to face such an emergency?
RQ3: Which measures did the University adopt to recover after the earthquake?
RQ4: How did the enrollment trend change after the earthquake?
RQ5: How did the students evaluate the role of Student Associations during the pre and post disaster phases?
Research design and data collection
This research combines multiple sources of evidences 24 and qualitative and quantitative analyses. Considering the first set of research questions, qualitative analysis aims at clarifying the earthquake impact on the University services and facilities, the emergency preparedness and the measures adopted to face the emergency (RQ1, RQ2, RQ3). To this purpose it was undertaken an evaluation of the various statistics published by the MIUR, the University of L’Aquila, and the newspaper articles. Quantitative analysis was applied to measure change in the enrollment trend (RQ4) and to assess students’ perception about the role that Student Associations played in the emergency preparedness and response (RQ5). Data published by MIUR were analyzed to assess the changes in enrollment trend, while a structured questionnaire administered to the students of the University of L’Aquila provided information to answer RQ5 and RQ6. The survey was carried out 3 months after the earthquake, adopting a non-probability convenience sampling 25. Students were approached at the campus of the college of Science (Coppito) in tents camp hosting the students coming from outside L’Aquila. The questionnaire was delivered with a drop-off pick-up methodology in order to reduce non-coverage error and possible sample bias. In addition, this methodology provides opportunities to gain experiential insights by having face-to-face contact with respondents 26,27. The questionnaire was anonymous and contained statements based on a five-items Likert Scale (1. Strongly disagree, 2. Disagree, 3. Uncertain, 4. Agree, 5. Strongly agree).
Results
The results of the study are presented in the following subsections:
– University’s services and facilities
– Emergency preparedness
– Recovery policies
– Enrollment trends
– Questionnaire
University services and facilities
The report of the structural engineering task force of the University of L’Aquila, which surveyed the status of facilities within the university precincts, revealed considerable damages 28. As a matter of fact, many buildings were highly vulnerable historical edifices. Indeed, many others were modern concrete frame structures with high seismic resistance. The historical buildings were affected by total or partial collapses; for example, the College of Literature (located in Palazzo Camponeschi), the College of Humanities (Palazzo Porcinari), the Rectorate and the administrative offices (Palazzo Carli), as well as the Conventions Center of San Basilio had been seriously damaged. The modern buildings (Engineering, Economics and Medicine) survived the shakes undamaged, while the College of Sciences reported very minor damages 28. The buildings stock was immediately declared unusable, teaching was suspended and many services interrupted. The students’ dormitory “casa dello studente” (the collapse of which caused 8 fatalities) and the various student lounges in Coppito were also closed. The emergency teams of the University were not on duty at the time of the earthquake and never activated. Except for the dormitories, which are under the jurisdiction of the Regione Abruzzo, the university is closed at night. Therefore the rescue operations were coordinated by the Italian National Department of Civil Protection with the support of the Police, the Army and the Firefighting brigades. A policy of “evacuate all” was adopted by the Civil Protection. The buildings were re-opened after thorough inspections performed by qualified engineers of the Civil Protection 29.
Emergency preparedness
According to the statute and regulations of the University l’Aquila, the Rector is the employer as defined by the 81/2008 Law Decree 8. The employer in an Italian organization/institution has major responsibilities and obligations to guarantee health, safety and security in the workplace. The University of L’Aquila Emergency and Safety Organization is shown in Figure 1. In such organigram, the Rector nominates a delegate for emergency and safety management who supervises and coordinates prevention and protection activities. This figure presides the Health and Safety Office – HSO (Area sicurezza ed igiene del lavoro), an office that belongs to the central university administration, which staff is under the direct dependency of the Administrative Director. The HSO deals with the regulations regarding the observance of the Italian Law on workers’ safety protection (e.g. biological, chemical, physics and carcinogenic agents protection; and equipment use). The HSO also deals with fire prevention, first aid, evacuation, health surveillance, and the disposal of harmful waste (e.g., radioactive, biological, toxic). The HSO also promotes the training and drills of the university personnel 30. At the operational level, in each primary structure, Colleges, Departments and Services, there is an Health and Safety Advisor, who, among other things, advises the heads of these primary structures on safety and security politics and strategies. The Health and Safety Advisor relates with the HSO and coordinates with other prevention and protection personnel (e.g. fire fighting, first aid, waste management).
Fig. 1: The University of L’Aquila Emergency and Safety Organization
Recovery policies
After the earthquake, the University gave a rapid response to mitigate the negative effects on teaching and institutional activities. Following is a discussion on goals and measures taken by the University to recover after the earthquake.
Right to education: two weeks after the earthquake, the classes restarted in the tensile structures set up by Civil Protection in Coppito. The College of Humanities benefitted of a temporary headquarter located in 3 buildings of the former Juvenile Court in the old town. This solution allowed to maintain the College in the original historical area. Since the academic year 2010/2011 this College was relocated at a former industrial facility in Bazzano, ans it is till waiting for a final destination. The College of Engineering was displaced in temporary campuses located in neighboring municipalities: Avezzano (57 Km from L’Aquila), Lanciano and Pineto, (respectively about 150 and 88 Km far from L’Aquila). During the academic year 2010/2011, Engineering was relocated in a new temporary campus at Campo di Pile (6 Km far from the old headquarter). Few months after the earthquake, the Rector and the professors decided to resume the teaching activities interrupted by the earthquake. E-learning options were activated and the European student exchange Programme Erasmus was encouraged by guaranteeing the extension of their scholarships. Italian colleges, research centers and various private companies offered hospitality in their laboratories to L’Aquila students. The College of Engineering gave its students the opportunity to complete their master thesis in other universities, e.g. Catania, Genova, Parma, Torino, which offered free hospitality in their dormitories to the students of L’Aquila. The damages suffered by the administrative facilities and the houses caused the loss of the academic transcripts, hence the University had to rebuild the students’ careers. The University could recover data only up to March 23, 2009, thus let the students reclaim the exams, they passed between March 24 and April 5, by presenting a written self-declaration, countersigned by the professors who administered the exams.
Dropouts mitigation: the University of L’Aquila introduced an incentive mechanism to lower mass migration to other universities and encouraged the recruitment by exempting the following categories of students to pay university fees for the academic year 2009/2010:
– Those enrolling in bachelor or master degree;
– Those renewing the enrollment in bachelor or master degree;
– Those moved from other universities to enroll in bachelor or master degree;
– Those enrolling in bachelor or master to obtain a second degree.
The agreement among the University of L’Aquila, the Regional Directorate of Transport of Abruzzi and the Civil Protection, allowed students enrolled at the University of L’Aquila to apply for free public transport. By mid November 2009, the University of L’Aquila received almost 4000 applications.
Psychological aid: in the days after the earthquake, the University opened a new section of the website dedicated to discussions about the disaster. Moreover, a section of the University website commemorates all the students who died in the earthquake (online at: https://www.univaq.it/ricordiamoli/index.html), while the College of Medicine and Surgery with the Rotary Club dedicated a memorial stone to dead students. Furthermore, in the months after the earthquake, each Faculty commemorated the dead students conferring them an honorary degree. On October 27th 2009, the University held a training course on earthquake safety in collaboration with the National Civil Protection, the Italian National Geophysical Institute – INGV and the National Firefighting brigades.
University facilities management: after April 6th 2009, the University modified the administrative organization better to cope with the seismic emergency and foster a rapid recovery. New administrative branches/offices were developed: i) Post-Earthquake Rebuilding Planning Office, ii) Earthquake Monitoring Centre, and iii) Aid Management Office. The Post-earthquake Rebuilding Planning Office was responsible to supervise the planning and reconstruction of old and new structures. In detail, this office verified the availability and provenance of external funding (dealing with sponsors), managed the bureaucracy related to construction and reconstruction, planned the final use of structures, and periodically reported to the central university administration the reconstruction progress. The Earthquake Monitoring Centre, is an observatory and research center that studies the earthquake phenomenon from different point of views, collecting data and evidences. This center aims at sensitizing the public on earthquake phenomena. Finally, the Aid Management Office to manage and coordinate donations that came from all over the world.
Enrollment trends
The office of statistics of the Ministry of Education (MIUR) publishes the annual enrollment data for Italian universities. Trends for first year enrollment and renewed enrollment at the University of L’Aquila were analyzed over the academic years 2004/2005 – 2011/2012. Data were aggregated to analyze trends for the whole university, and split to show differences among the three campuses. Before the earthquake, the Colleges Humanities, Sport Science, Education, and Psychology were located downtown/Centro, the Colleges of Medicine and Surgery, Biotechnology and Mathematics Physics and Natural Science, were located at the Coppito Campus, whereas the College of Engineering and Economics were located at the Roio Campus. Students were distributed as follows: Centro (36.8%), Coppito (33.3%), Roio (29.9%). Over the five years term before the earthquake, the University of L’Aquila had a steady year-by-year increase (Fig. 2). The earthquake of April 2009 produced a relatively small decline (-4.7%) for the first year enrollment, but left unchanged the renewed enrollment for academic year 2009/2010. The lost for the first year enrollment was distributed evenly among the three campuses. The Colleges that reported the most significant decline were Biotechnologies (-46.7%) and Engineering (-25.7%). On the contrary, the Colleges that recorded important boost for the first year enrollment were Economics (46.9%) and Education (26%). As said above, the renewed enrollment for academic year 2009/2010 at the University of L’Aquila was substantially unchanged (Fig. 2). The College that recorded the worst decline in renewed enrollment was Biotechnologies (-15.3%). See Table 1.
Table 1: Change in enrollment (%) between 2008/’09 A.Y. and 2009/’10 A.Y.
Fig. 2: a) Total enrollment ; b) First year enrollment; c) Renewed enrollment
Questionnaire
Demographic profile of the respondents. A total of 110 students answered the questionnaire, 49% of which were females. Their age ranged between 19 and 41 (24.1±3.35). The distribution among the various colleges of the respondents were as follow: College of Mathematics, Physics and Natural Science (28%), Humanities (27%), Medicine and Surgery (22%), Engineering (9%), Psychology (5%), Sport Science (4%), Biotechnologies (3%), Economics and (1%) Education Science (1%). In other words, 53% of respondents were from the Coppito Campus, 37% from Centro, and 10% from the Roio Campus. The percentage from Centro is in line with enrollment data, whilst Coppito and Roio campuses are slightly overestimated and underestimated respectively.
The role of the Student Associations in pre and post-disaster phases.
Considering the long lasting seismic swarm that affected the area before the main-shock, interviewed students were asked whether they agreed with the following statement: “Student Associations asked the university administration to verify the structural integrity of the university facilities (classrooms, dorms, and recreational areas).” About 45% of respondents disagreed or totally disagreed, 34% stated otherwise, and about 21% was uncertain. Students were asked whether they thought that Student Associations tried to raise awareness on seismic risk before the earthquake occurred. About 74% of the respondents totally disagreed and 7% disagreed, while 14% agreed. When asked what type of activities were put in place, the following were detailed: leafleting (43%), social networks campaigns (36%), meetings (7%), demonstrations (7%) and drills (7%). The majority of respondents (58%) considered Student Associations a suitable and effective channel to discuss and raise awareness about seismic risk. A similar percentage (59%) affirmed that Student Associations played a pivotal role in reigniting campus life. The totality of the interviewed students claimed that Student Associations did not have a plan to deal with a possible seismic emergency, yet 95% of respondents ignored the emergency plan prepared by the University. Moreover, 75% of the students did not know the existence of external Student Associations (e.g. LARES from Perugia) that came in support to students during the post-emergency phases, and 61% of them ignored the services provided to the University by local Citizen Groups purposely created to deal with the seismic emergency. Among those who knew of the external associations, a small percentage (32%) could specify the role played by these associations during the recovery. Only 2% of the respondents took part to the activities performed by the Student Associations. Results of the psychometric tests are summarized in table 2. The inferential analysis highlighted some patterns: Mann Whitney U test revealed a significant difference in the perception of respondents who knew about Citizen Groups’ activities (Mdn=4) and who did not (Mdn=3) to the statement number 1 (Tab.2), U=537, p<0.05, r=-.23. Similarly, respondents who knew about the external associations (Mdn=4) were more likely to agree to statement number 1 (Tab.2), when compared to those who did not know (Mdn=4), U=498, p<0.05, r=-.19. Regarding the knowledge of the university emergency plan, respondents who knew the plan were more likely to agree to statement number 1 (Mdn=4) – (U=141.5, p<0.05, r=-.22), and statement number 2 (Mdn=4) – U=22, p<0.001, r=-.48, when compared to those who did not know (Mdn=4 and Mdn=4 respectively). Finally, people who knew about Citizen Groups’ activities were almost three times more likely to know about external Student Associations operating during the emergency, χ2(1)=4.06, p<0.05, Φ=.23.
Results of the psychometric tests (five-items Likert scale statements)
Statements
1. Strongly disagree
2. Disagree
3. Uncertain
4. Agree
5. Strongly agree
1. Student Associations asked the administration to verify the structural integrity of university’s facilities
41%
4%
21%
14%
20%
2. Student Associations got active to raise awareness of seismic risk before the earthquake occurred
74%
7%
5%
8%
6%
3. Student Associations are a suitable and effective channel to discuss and create care about seismic risk
22%
6%
14%
20%
38%
4. Student Associations played a pivotal role in the recovery of the campus life
16%
6%
19%
45%
14%
Discussion
The earthquake of April 6th 2009 hit the facilities of the University of L’Aquila causing the death of 55 students and massive infrastructural damages. Despite the high seismicity of the territory and a long seismic swarm (which begun in October 2008), the University was caught unprepared to cope with the disaster, and the offices accountable for prevention and protection did not disseminate or made known any emergency plan. Nonetheless, because the disastrous earthquake happened at night, the Health and Safety Office, responsible to manage the first response in emergency was not operational (such office had not recovery and business continuity functions). After the disaster, the Rector and the administrative staff worked very hard to mitigate the medium and long-term impact on the University of L’Aquila. Teaching activities were resumed 15 days after the earthquake, thanks to the support of the National Civil Protection, which provided the tensile structures used as classrooms. Moreover, the Declaration of the State of Emergency streamlined the bureaucracy, enabling a fast reorganization of temporary campuses. The Roio campus was relocated in the coastal cities of the “Regione Abruzzo.” The university had to rebuild the students’ careers due to the loss of the academic transcripts (the lack of a data protection and redundancy systems was fairly surprising). Even so, the policies adopted by the University curbed students’ migration; some major tax waivers, and other economic benefits, convinced students not to leave and continue their studies at the University of L’Aquila. The students’ dropout ratio for the academic year following the earthquake was correlated to the dropout of first year enrollment; the renewed enrollment was pretty much unchanged. All that said, it is remarkable to notice that the measures taken by the university administrators were based on an “ad hoc” strategies as no emergency and continuity plans were prepared in advance. As Alexander 31 pointed out, in Italy efforts to avoid the catastrophic consequences of extreme events have almost always been limited to therapeutic actions, rather than on pre-disaster preparedness planning. Indeed, this case study of the University of L’Aquila confirmed such cultural attitude. In regard to the role of Student Associations, perhaps the best proxy to assess their accomplishment, was the 2012 elections to renew the boards of representatives of such associations at the University of L’Aquila. Circa 22% of the students expressed their vote in such election; a good result considering that the average turnout at national level is way less than 20%. This good participation could reflect the trust gained by Student Associations during the emergency. Although, truth to be said, neither these associations planned appropriate disaster risk reduction activities. As with the University administration, the Student Associations at L’Aquila became active during the recovery and restoration activities, but did very little with emergency preparedness and risk awareness programs before the earthquake.
Conclusions
Italy lacks a culture of disaster prevention and preparedness and relays mostly on adaptive tactics rather than on strategic planning to face emergencies. The case of the 2009 L’Aquila earthquake confirm this state of affairs. The university of L’Aquila lacked a pre-disaster mitigation and recovery plan and only a small portion of students knew some emergency procedures. The information, training and drill activities were not enough to produce an acceptable level of emergency preparedness among students. Indeed, Universities may potentially represent a fertile ground to promote a culture of safety and stop this trend. Greater awareness and involvement should be pushed forward at each level (administrators, faculties, students) to plan in advance for adverse scenarios, and to make steps toward the development of a culture of safety in Italy. Further discussion and research on Universities’s emergency preparedness is necessary, also better to clarify the role that Student Associations may play to support and spread a culture of prevention and safety.
Corresponding Author
Michele Magni: [email protected]
Data Availability
Data can be accessed at: https://figshare.com/projects/Emergency_preparedness_and_management_at_the_University_of_L_Aquila/17759
Competing Interest
The authors have declared that no competing interests exist.
Methods: We conducted a retrospective observational study to determine the prevalence of hypertension among patients seeking medical care at mobile medical clinics after Typhoon Haiyan in the Philippines.
Results: A total of 3,730 adults were evaluated at the mobile medical clinics. Analysis of the medical records revealed that the overall prevalence of hypertension among adult patients was 47%. Approximately 24% of adult females and 27% of adult males were classified with stage 2 Hypertension.
Conclusions: Evidence-based guidelines on the management of hypertension and other NCDs (diabetes mellitus, cardiovascular disease, chronic lung disease and mental health) during humanitarian emergencies are limited. Clinical care of victims of humanitarian emergencies suffering with NCDs should be a critical part of disaster relief and recovery efforts. We therefore recommend the development of best practices and evidence based management guidelines of hypertension and other NCDs in post-disaster settings.
]]>Introduction
On November 8, 2013, Super Typhoon Haiyan struck the Philippines resulting in 6,000 deaths and the displacement of 3.4 million people, a humanitarian emergency. Samaritan’s Purse (SP), a faith based organization, responded to the appeal by the Philippine Department of Health for international assistance. Partnering with the Schistosomiasis Control and Research Hospital (SCRH) in Palo, Leyte, SP established and staffed a Type 1 field hospital (WHO 2013; “Minimum Standards for Foreign Medical Teams) in the parking lot of this heavily damaged hospital. In addition to providing acute medical care for the residents of the city of Palo, SP’s hospital served as a base of operations for mobile medical teams (MMTs) that deployed daily to remote locations. Essential health services were provided to residents in 40 barangays (smallest administrative division in the Philippines and is the native Filipino term for a village, district or ward) in remote and otherwise unreached areas on the islands of Leyte and Samar. Prior to Typhoon Haiyan, residents in the barangays typically accessed Barangay Health Services (BHS) for health care. After the typhoon, the death of healthcare workers and the destruction of transportation infrastructure led to the disrupted access to healthcare services.
According to the World Health Organization, non-communicable diseases (NCDs), also known as chronic diseases, are the leading cause of death and disability around the world. The four main types of non-communicable diseases are cardiovascular diseases, cancers, chronic respiratory diseases (such as chronic obstructed pulmonary disease and asthma) and diabetes; we will be referring to these four diseases in our paper. NCDs kill 38 million people each year. Sixteen million NCD deaths occur before the age of 70; 82% of these occurred in low- and middle-income countries1 . Healthcare systems are often disrupted in post-disaster situations, reducing access to care and medications, which can lead to exacerbation of NCDs2 . Literature on post-disaster morbidity and mortality among persons suffering from NCDs and management of NCD during humanitarian emergencies is limited3 .
In 2007, the 15th World Congress on Disaster and Emergency Medicine, held in Amsterdam, recommended that health outcome assessments of disasters, incorporate NCDs as a factor affecting the health challenges in a population4. Even so, humanitarian actors seldom address NCDs specifically or assess their impact. This may be because the acute needs of those with traumatic injuries consume available resources, and acute medical issues in mass casualty events capture the focus of responders. Disregard of the medical needs of persons with NCDs can add to the toll of suffering resultant from the catastrophe. The lack of literature on NCDs in disasters points to a need for further investigation into the care of those with NCDs during humanitarian emergencies5.
More information on the extent and nature of the issue could facilitate better planning and preparation by humanitarian agencies seeking to address the overall morbidity and mortality associated with traumatic events. This report presents a post disaster evaluation of the burden of hypertension among victims of Super Typhoon Haiyan in the Philippines.
Methods
A retrospective observational study was completed in order to determine the prevalence of hypertension among patients attending clinics conducted by mobile medical teams (MMTs) in 40 barangays located in central Leyte and Western and Eastern Samar, island provinces within the Philippine Archipelago. Medical records were kept for all patients. Patient evaluations included a history and physical, during which vital signs were measured and recorded. Blood pressure readings were taken using sphygmomanometers and stethoscopes. Results were recorded in patient medical records as systolic/diastolic pressure expressed as millimeters of mercury (mmHg). These results were then entered into an electronic patient database.
Causes of morbidity were documented and submitted daily to the Department of Health of the Philippines utilizing that department’s “Surveillance in Post Extreme Emergencies and Disasters” (S.P.E.E.D.) forms.
The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI) defined and classified hypertension in adults, as systolic BP ≥140 mm Hg and diastolic BP ≥ 90 mm Hg6. Stage 1 Hypertension is defined as a systolic pressure ranging from 140 to 159 mm Hg or a diastolic pressure ranging from 90 to 99 mm Hg. Stage 2 Hypertension is defined as a systolic pressure of 160 mm Hg or higher, or a diastolic pressure of 100 mm Hg or higher. For the purpose of this study only adult patients, those 18 years old or older, were included.
Ethical approval was obtained from the Philippines Ministry of Health, Regional Office VIII, Leyte, Philippines.
Results
The top three diagnoses among adult patients were: a) acute respiratory illness (with or without bronchospasm and associated complications), b) hypertension (HTN), and c) puncture wounds requiring tetanus immunization as well as those complicated by infection. Clinical care was provided to a total of 3,730 adults, including 1,020 males and 2,710 females. Of these, blood pressure (BP) results were available on 986 males and 2,647 females for a total of 3,633 adults. The male to female patient ratio approximated 1:3. The mean age of adult patients was 50.4 ± 17.1 years (Table 1).
Analysis of the medical records from all clinic visits revealed that the overall prevalence of hypertension among adult MMT clinic patients was 47% (47 per 100 individuals). In 34 out of the 40 barangays more than 40% of patients had BP readings consistent with a diagnosis of hypertension. Hypertension was especially prevalent in the following barangays (district): New Kawayan, Rizal Dagami, Guinan Cogdara-o, Basay, Bugho, Basey Balud, Roxas and Tigbaw (Figure 1).
Further analysis of BP readings from adult patients seeking care through an MMT clinic revealed that 22.2% exhibited stage 1 Hypertension (S1HTN) and 24.9% presented with stage 2 Hypertension (S2HTN). Stratified by gender, 22.7% of males presented with S1HTN and 26.6% had blood pressure readings consistent with S2HTN. Among female patients 22% had S1HTN while 24.2% exhibited S2HTN (Table 2).
Discussion
A retrospective review of the medical records of MMT clinic adult patients revealed that the most common reason given for their seeking care was for treatment of acute respiratory illness followed by hypertension. Our study had several limitations. We did not collect socio-demographic data such as obesity, smoking status, hypercholesteremia, etc. Second, we were not able to evaluate end-organ damage.
There were fewer adult males compared to adult females attending MMT clinics. The need to rebuild and rehabilitate devastated infrastructure, as well as earn a wage to sustain their families, made it difficult for working male adults to access medical care. Among the males seeking care through an MMT clinic, a high percentage exhibited either Stage 1 or Stage 2 hypertension, although hypertension was rarely their primary reason for seeking care.
We selected antihypertensive therapy from Standard Treatment Guidelines used in the Philippines, which were administered at conservative doses to achieve blood pressure control. Anticipating that the Filipino Department of Health would be recovering for a protracted period, temporary measures were implemented to bridge gap for hypertension management. A 10 to 30 day supply of medications was dispensed in anticipation of restoration of health services. Patients with a previous diagnosis of hypertension often reported decreased access to medicine as a result of the typhoon. With approval by the Filipino Department of Health and local leaders, SP attempted to bridge the gap in the acute phase post-disaster by distributing of sphygmomanometers and related equipment, along with antihypertensive medications, for future use by local healthcare workers and rural health units. It is recommended that all NGOs that have a health response during a disaster work closely with the Ministry of Health to ensure the sustainability of chronic disease management during the recovery phase.
Patients with hypertensive urgency and who were symptomatic (neurological changes, associated headache, chest pain, etc.) were referred to a functioning hospital that had not been seriously impacted by the typhoon. When warranted, assistance with transportation was provided to the closest health care facility. Interim medical supply chains may be required to bridge healthcare needs while medical infrastructure is reestablished. With that in mind, it is paramount that humanitarian actors work in coordination to extend and maximize temporary availability of medical supplies and services to address NCDs.
The prevalence of hypertension among this patient population was likely impacted by diarrheal diseases and dehydration secondary to the lack of access to potable clean water frequently seen in the aftermath of a disaster. In patients with a known diagnosis, the most common reason for seeking care was acute respiratory illness.
Previous studies in post-disaster settings have reported that blood pressure in some individuals, confounded by anxiety and post-traumatic stress, may remain abnormally elevated for months7,8,9,10. While it is possible that patients with a known history of hypertension may be slightly over represented in relief health services to obtain medication refills, the overall experience in the MMT clinics did not support this as the motivation for care-seeking behavior after Typhoon Haiyan. As previously noted there were fewer adult males compared to adult females attending MMT clinics. The need to rebuild and rehabilitate devastated infrastructure, as well as earn a wage to sustain their families, made it difficult for working male adults to access medical care. Among the males seeking care through an MMT clinic, a high percentage exhibited either Stage 1 or Stage 2 hypertension.
Preyson 3, a prospective, multi-staged, stratified nationwide survey on hypertension found that the prevalence of hypertension in the Philippines was 28%11. Among those with NCDs, the majority of patients presented with elevated blood pressure. The prevalence of hypertension in a population cluster sample of displaced persons in shelters after hurricane Karina was found to be 34%, while the prevalence of hypertension among victims of the Wenchuan earthquake in China was 24%12,13. The prevalence of hypertension in China in this population was similar to the prevalence prior to the earthquake (27%). The population of displaced person after hurricane Katrina likely had chronic hypertension and it is not clear whether the prevalence of hypertension increased in the aftermath of Katrina.
A surprising 47% of the adult population evaluated at our MMT clinics exhibited evidence of elevated blood pressure; though it’s not clear if this was secondary to chronic disease or just elevated due to stress in the post-disaster setting. Unfortunately, patient reporting of pre-disaster medical history was not always reliable. Patients with a previous diagnosis of hypertension often reported decreased access to medicine as a result of the typhoon as a reason for care seeking. Had the disaster happened in a community with more complete medical records, we would be able to determine more accurately what percentage of the hypertension or elevation in pressure was due to stress secondary to disaster-related factors.
Typically, hypertension guidelines recommend that systolic and diastolic blood pressure be reduced to values less than 140/90 mm Hg and that control for patients with hypertensive urgency be achieved conservatively over hours or days14. Some studies suggest that management of hypertensive urgency (even in the short term) could be clinically beneficial. Unaddressed hypertensive urgency not only increases the risk of cardiovascular and cerebrovascular events, but also the progression towards end organ damage15.
There is evidence to suggest that tight control of hypertension is beneficial and can reduce cardiovascular outcomes16. In the Cardio-Sis trial, where patients were randomized to tight versus usual control, it was found that new-onset atrial fibrillation and coronary revascularization occurred less in the tight-control group. However, the incidence of myocardial infarction, admission for heart failure, stroke, transient ischemic attack, and all-cause mortality was low and did not differ between the groups16. It is important to note that the follow-up period was two years for this study and therefore might not be applicable to this particular setting. It is not clear if treating hypertension for a few weeks will result in significant changes in cardiovascular outcomes in the long run. In protracted conflicts such as the Syrian crisis, these results would perhaps be more relevant.
In a post-hoc analysis of the Cardio-Sis trial, the risk of composite cardiovascular end point was higher in the group with cardiovascular disease at baseline than in the group without17. The risk of cardiovascular outcomes was also lower in patients assigned to the tight control than in those in the standard BP control group. The benefits of controlling hypertension with respect to stroke, renal, and cardiovascular disease complications led international guidelines to recommend reduction of BP to <140/90 mm Hg for uncomplicated hypertension or <130/80 mm Hg for subjects with co-morbid kidney or cardiovascular disease17. However, it is less clear whether adverse outcomes will occur in the setting of non-compliance in the short-term, or whether tight control is beneficial in a post-disaster setting.
Several studies have shown an increase in mortality secondary to cardiac causes following an earthquake18,19,20,21,22,23. One such study conducted in Japan following the Hanshin Awaji earthquake in 1995, postulates that increased hypertension contributed to a threefold increase in myocardial infarction among populations in close proximity to the earthquake, particularly in women, and a near doubling in the frequency of strokes23. Hypertension is known as the single most important risk factor for ischemic strokes. It is seen in 75% of patients with acute ischemic stroke, in 80% of patients with acute intracerebral hemorrhages, and is independently associated with poor functional outcome24. Unaddressed hypertensive urgency not only increases the risk of cardiovascular and cerebrovascular events, but also the progression towards end-organ damage.
It would therefore be important to have cohort studies in place that would be able to track outcomes following a disaster. The importance of prospective cohort studies that are able to evaluate both short and long-term outcomes following a disaster is paramount. In hypertensive urgency (≥180/≥110 mm Hg), the absence of clear clinical events at the time of a disaster (such as stroke, renal failure, or a myocardial infarction) makes it difficult to understand the impact of treatment interruption in the short-term.
Our study is relevant as it contributes to the body of literature on the burden of hypertension in the post-disaster period. Further studies are needed to determine blood pressure targets for victims of disasters who do not have access to treatment in the aftermath of a disaster. Additionally, it is important to understand whether patients that are at high risk of developing negative outcomes, such as those with concomitant kidney disease and cardiovascular disease, require more tight control of their blood pressure. It is important to develop better guidelines that provide more detailed recommendations on blood pressure targets, on the optimal use of drugs to treat hypertension (especially when one does not have appropriate follow-up) and groups that require tight control.
It is recommended that other NGOs that have a health response during a disaster disasters work closely with Ministries of Health to ensure the sustainability of chronic disease management during the recovery phase. Without this partnership, access to medicines and services required to manage NCDs will remain a challenge.
Conclusions
Better planning and preparation by humanitarian actors seeking to decrease the overall morbidity and mortality associated with disasters should include treatment of NCDs. There is limited evidence regarding the optimal management of hypertension in disaster settings. Clinical care of patients with hypertension and other NCDs is an important part of disaster relief and recovery. We recommend future studies to determine best practices and evidence-based management of other NCDs (such as diabetes mellitus, cardiovascular disease, chronic lung disease, mental health etc.) in post-disaster settings.
Competing Interests
The authors have declared that no competing interests exist.
Data Availability
Data are available in Figshare at https://figshare.com/s/adcd8bc96bd0164cc107
Corresponding Author
Dr. Linda Mobula: [email protected]
Methods:Generalist humanitarian healthcare responders, including both physicians and nurses, were trained in ultrasound guided femoral nerve block (USGFNB) and landmark guided fascia iliaca compartment block (LGFICB) techniques using didactic sessions and interactive simulations during a one-day focused course. Outcome measures evaluated interval knowledge attainment and technical proficiency in performing the RA procedures. Knowledge attainment was assessed via pre- and post-test evaluations and procedural proficiency was evaluated through monitored simulations, with performance of critical actions graded by two independent observers.
Results:Twelve humanitarian response providers were enrolled and completed the trainings and assessments. Knowledge scores significantly increased from a mean pre-test score of 79% to post-test score of 88% (p<0.001). In practical evaluation of the LGFICB, participants correctly performed a median of 15.0 (Interquartile Range (IQR) 14.0-16.0) out of 16 critical actions. For the USGFNB, the median score was also 15.0 (IQR 14.0-16.0) out of 16 critical actions. Inter-rater reliability for completion of critical actions was excellent, with inter-rater agreement of 83.3% and 91.7% for the LGFICB and USGFNB evaluations, respectively.
Discussion:Prior to conducting a trial of RA in a disaster setting, providers need to gain understanding and skills necessary to perform the interventions. This evaluation demonstrated attainment of high knowledge and technical skill scores in both physicians and nurses after a brief training in regional anesthesia techniques. This study demonstrates the feasibility of rapidly training generalist humanitarian responders to provide both LGFICB and USGFNB during humanitarian emergencies.
]]>Notice of Correction
6 February 2017: PLOS Currents – Correction: Aluisio AR, Teicher C, Wiskel T, Guy A, Levine A. Focused Training for Humanitarian Responders in Regional Anesthesia Techniques for a Planned Randomized Controlled Trial in a Disaster Setting. PLOS Currents Disasters. 2016 Nov 16 . Edition 1. doi: 10.1371/currents.dis.e75f9f9d977ac8adededb381e3948a04. View Correction.
Background
Between 1994 and 2013, approximately 7000 natural disasters were reported, affecting more than 200 million people and accounting for over one million deaths globally. Among geophysical disasters, earthquakes result in high mortality rates and account for the largest burden of injuries1,2. Research from multiple settings demonstrates that earthquake-associated trauma most commonly causes injuries to the lower extremities3,4,5,6. Inadequate pain management during natural disasters, where resources are often constrained, is common and can result in both short-term and long-term physiologic and psychological sequela among an already high-risk patient population7,8,9,10.
Prior studies have demonstrated that regional anesthesia (RA) is a rapid and safe method for reducing pain caused by lower extremity trauma, and as such may have a role in improving pain management during the acute response phase of a major earthquake11,12,13,14,15. However, most studies on RA have been conducted in high-resource settings by specially trained proceduralists and have only enrolled patients with simple hip or femur fractures, which may not be generalizable to the more complex injury pattern typical of earthquake-related trauma16,17,18. There are anecdotal reports of the use of both landmark guided (LG) and US-guided (USG) RA for treatment of earthquake-related injuries, suggesting feasibility in the use of these modalities in disaster settings9,19,20. However, there have been no high-quality studies conducted evaluating the effectiveness, safety, or acceptability of RA in the aftermath of a major earthquake.
The Regional Anesthesia for Painful Injuries after Disasters (RAPID) study is randomized controlled trial (RCT) that will be carried out in the immediate aftermath of a major earthquake to determine whether RA provided by generalist humanitarian medical responders, either with or without ultrasound-guidance, can improve pain treatment for lower limb injuries, above current standards of care21. The RAPID study will be implemented by Médecins Sans Frontières (MSF) personnel deployed in response to an earthquake in a low- or middle-income countries (LMIC) setting21,22,23. Limited prior research on training non-specialist providers in RA in pre-hospital and emergency department settings has demonstrated successful skill attainment24,25,26,27. Although this evidence supports the concept of generalist humanitarian providers being capable of performing RA, no data exists pertaining specifically to this population, who provide care in unique practice environments. This study assesses knowledge translation and skill acquisition for simulated lower extremity RA performed both with and without ultrasound guidance by a cohort of MSF association members and describes the focused training methodology used.
Methods
Ethics
The RAPID study has received ethical approval from the Médecins Sans Frontières Ethical Review Board (Reference number: 1524) and has been preregistered at ClinicalTrials.gov (number: NCT02698228)21. All training participants provided written informed consent for study activities which were conducted in accordance with the Declaration of Helsinki.
Study Design Setting and Population
This cross-sectional study was designed to evaluate the efficacy of a focused training in regional anesthesia for lower extremity injuries provided to MSF volunteers who will serve as research proceduralists in a future RCT of RA for pain management in earthquake victims21. Study activities were carried out during a one-day training in June of 2015 at the MSF-USA office (New York City, United States).
The study population was comprised of physician and nurse responders who had previously been deployed to humanitarian emergencies and were members of the MSF-USA association. Participants were made aware of the RAPID study and training prior to the meeting via digital correspondence with study investigators and were solicited to volunteer for participation.
Participant Training and Assessment
Training activities were designed to provide understanding of RA principles and competence in performing landmark guided fascia iliaca compartment blocks (LGFICB) and ultrasound-guided femoral nerve blocks (USGFNB). Study throughput is outlined in Figure 1. Participants completed a baseline knowledge assessment prior to the provision of training activities. The pre-assessment was comprised of fifteen multiple-choice questions that covered topics pertaining to techniques for general RA and specifically to LGFICB and USGFNB. Training and assessment materials were derived from joint committee recommendations for education and training in ultrasound-guided interventional pain procedures from American, European and Australasian international pain and anesthesia societies28. Participants were randomly allocated to take one of two versions of the assessment exam (test A or test B), with each exam having fifteen questions which were unique in both query stems and possible responses but which covered the same content matter and key concepts.
Following the initial assessment, participants took part in a three-hour interactive didactic session lead by study investigators using a semi-structured discussion platform that allowed for open-form content exchange between all participants. The educational information focused on RA principles and specific methodologies in performing LGFICB and USGFNB28. Additional information relating to the RAPID study protocols was also provided. Given the evidence supporting the use of simulation in teaching invasive procedures29, participants took part in three simulation-based training sessions subsequent to the didactic session. These three sessions focused on performance of USGFNB, LGFICB and general ultrasound-guided needle injection. The duration of each practical session was 45 minutes, with a 3:1 participant to instructor ratio in each session. All instructors were board certified physicians in either anesthesia or emergency medicine or senior emergency medicine residents with experience in RA techniques. The LGFICB sessions were taught using a live model simulation with a focus on surface anatomy and technical aspects specific to the procedure. For the USGFNB sessions, a femoral regional anesthesia ultrasound model (CAE Healthcare™, model number: BPF1400) was used, focusing on technical aspects of the procedure specific to perineural anesthetic delivery. For the ultrasound-guided needle injection training, regional anesthesia ultrasound training block models (CAE Healthcare™, model number: BPNP150) were used and participants were able to perform multiple injections and practice needle control and delivery under ultrasound guidance with instructor support. All ultrasound trainings and evaluations were performed using Sonosite Edge™ and Terason uSmart™ 3200T ultrasound machines with high-frequency 6-13MHz linear transducers.
After completion of training activities, each participant was assessed through two observed simulation exams for performance of the LGFICB and the USGFNB. In each exam, participants were asked to perform the RA techniques using standard clinical equipment and a femoral regional anesthesia ultrasound model (CAE Healthcare™, model number: BPF1400). During the simulation exams, two independent reviewers assessed each participant’s technical competency using a preformed critical actions checklist with an objective scoring system. Assessed parameters evaluated appropriate positioning; identification of anatomic and ultrasonographic landmarks; use of sterile technique; provision of local superficial anesthetic; needle delivery; anesthetic injection; and proper procedural monitoring for possible adverse events.
A post-training, fifteen question multiple-choice exam was performed to assess interval knowledge attainment. In the post-training assessment, participants were crossed-over to complete the alternative exam to the one they took at baseline (i.e., those initially allocated to test A completed test B and those which started with test B completed test A).
Data Collection Outcome Measures
Baseline data on participants was collected using a structured questionnaire. Information on demographics, healthcare training, humanitarian response activities, ultrasound and RA experience was gathered. Knowledge assessment exams were scored with a single best answer for each question and participants were assigned a percent correct for both the pre-test and post-test. During observed simulation exams for the RA techniques, each rater provided a critical action completion score ranging from zero to sixteen based on eight assessment parameters. Accrued data was de-identified and entered into a password-protected database that was accessible only by study personnel.
The primary outcome measures were the change in knowledge attainment based on mean pre- and post-test scores on the standardized exams and demonstration of technical competency in performing the LGFICB and USGFNB RA techniques. Technical competency was assessed based on adequate performance of critical actions during simulation assessments. Secondary outcome measures included the inter-rater reliability for the standardized critical action checklist and separate subgroup analyses of physician and nurses.
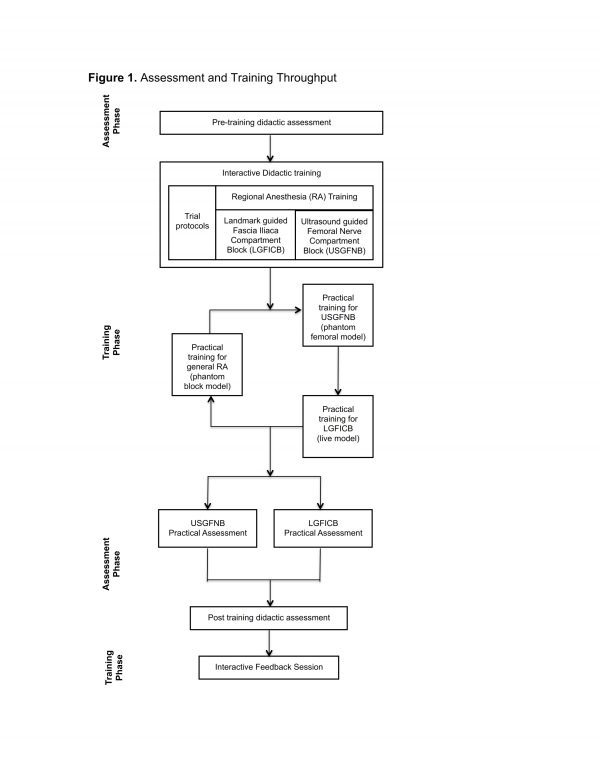
Fig. 1: Assessment and Training Throughput
Statistical Analysis
Statistical analyses were performed using STATA 13.0 (StataCorp LP, College Station, USA). Characteristics of the cohort were evaluated using descriptive methods. Categorical variables were explored using frequencies with percentages, and continuous variables were analyzed using medians with corresponding interquartile ranges (IQR) or means with associated 95% confidence intervals (95% CI). Given the small sample size knowledge attainment data was analyzed using Shapiro-Wilks tests and frequency distributions to evaluate for normality. The results were found to satisfy criteria for normality and as such, one sample paired t-tests were used for the primary outcome of change in mean knowledge scores. A p value less than 0.05 was considered significant in primary outcome assessments.
Median scores with IQR for each rater were calculated for the LGFICB and USGFNB simulation assessments. Inter-rater reliability (IRR) was evaluated across all critical assessment variables based on rater agreement derived using Cohen’s kappa calculation. Kappa values were interpreted according to previously utilized criteria with agreement classified as greater than 0.80 as representing excellent IRR30,31. Stemming from inherent difference in healthcare training and practice roles, outcomes for the cohort were stratified and analyzed based on participants’ professional training as a nurse or physician. Subgroups were compared using independent sample t tests or Mann-Whitney U tests for normally and non-normally distributed variables respectively. To account for multiple testing, a Bonferroni correction was utilized and a significance level of less than 0.008 was used for stratified analyses32.
Results
Twelve MSF association members were enrolled and all participants completed the full study training and assessment procedures. The median age of the cohort was 41 years and the majority of participants were female. Half of participants reported their primary healthcare training as nurse and half as physician. The median years of healthcare practice and humanitarian response experience were eleven and five years respectively. Half of the cohort had prior experience with ultrasound use, though only a minority reported previous clinical application of RA techniques (Table 1).
* MSF abbreviates Médecins San Frontières
Characteristics
n (%) / Median (IQR)
Age (years)
41 (35, 48)
Sex
Male
2 (16.7%)
Female
10 (83.3%)
Primary healthcare training
Nures
6 (50.0%)
Medical Doctor
6 (50.0%)
Duration providing healthcare (years)
11 (10, 21)
Duration as MSF* response personnel (years)
5 (3, 9)
Number of response missions performed with MSF*
4 (4, 7)
Prior clinical use of ultrasound
No
6 (50.0%)
Yes
6 (50.0%)
Prior clinical use of regional anesthesia
No
10 (83.3%)
Yes
2 (16.7%)
The primary study outcomes are summarized in Table 2. Training activities resulted in a significant increase in mean knowledge assessment scores of 9.2% (p<0.001). The mean pre-training and post-training scores were 79.2% and 88.4%, respectively. Median values for achieved critical actions during simulation assessments were all greater than or equal to 15 as scored by the independent raters. Overall an excellent degree of IRR was observed between rater evaluations for the simulated RA assessments. The IRR agreement for technical assessments of the LGFICB and USGFNB were 83.3% and 91.7% respectively (Table 2).
* Values represent the percent mean score with associated 95% confidence intervals (95% CI), # LGFICB abbreviates landmark guided fascia iliaca block and USGFNB abbreviates ultrasound guided femoral nerve block, † Reported as median score with associated interquartile range (IQR) out of possible score of sixteen required critical actions
Pre-training
Post-training
Percent Change
p
Didactic Knowledge assessment score*
79.2 (73.9-84.4)
88.4 (82.3-94.2)
9.2%
<0.001
Rater 1†
Rater 2†
Kappa
–
LGFICB assessment#
15.0 (14.0, 16.0)
15.0 (15.0, 16.0)
0.83
–
USGFNB assessment#
15.0 (14.0, 16.0)
15.5 (14.5, 16.0)
0.92
–
Table 3 demonstrates stratified outcome assessments based on participants’ healthcare training. There were no significant differences identified in knowledge attainment or technical skill performance between the physician and nurse subgroups.
* Values represent the percent mean score with associated 95% confidence intervals (95% CI), # LGFICB abbreviates landmark guided fascia iliaca block and USGFNB abbreviates ultrasound guided femoral nerve block, † Reported as median score with associated interquartile range (IQR), maximum possible score out of sixteen required critical actions
Assessment Type
Nurse
Physician
p
Pre-training didactic exam*
78.7 (74.3-83.1)
79.6 (67.6-91.7)
0.86
Post training didactic exam*
91.7 (85.6-97.8)
85.2 (73.7-96.1)
0.23
LGFICB assessment#
Rater 1†
14.5 (14.0, 15.0)
14.0 (14.0, 16.0)
0.18
Rater 2†
15.0 (14.0, 16.0)
15.0 (15.0, 16.0)
0.06
USGFNB assessment#
Rater 1†
15.5 (15.0, 16.0)
14.0 (14.5, 16.0)
0.35
Rater 2†
15.5 (14.0, 16.0)
15.5 (15.0, 16.0)
0.80
Discussion
This study assessed knowledge translation and skill acquisition outcomes for simulated lower extremity RA performed both with and without ultrasound guidance among a small cohort of MSF volunteers who will function as proceduralists in a planned randomized controlled trial that will assess the efficacy of RA for pain management in the acute phase of a major earthquake21. The results demonstrate high knowledge and technical skill acquisition with good agreement between independent raters. These findings illustrate success of the focused training methods used in this population of response providers in gaining proficiency in both LGFICB and USGFNB regional anesthesia.
In the acute response phase to a natural disaster, where resources are often constrained, oligoanalgesia is common7,8,9. Standard pain management in disaster settings for severe lower limb injuries focuses on the use of parenteral narcotic medications33,34. However, such medications are frequently unavailable creating preexistent barriers to analgesic treatment in low-income disaster settings35,36. Additionally, even when narcotic medications are accessible patients with trauma often have tenuous hemodynamic states, making administration of narcotics clinically unfavorable, especially in situations where continuous cardiorespiratory monitoring and personnel are limited. Subsequently, insufficient pain management can potentiate both short-term and long-term sequela, including immunosuppression, thrombotic complications, posttraumatic stress disorders, and chronic pain syndromes, further increasing the morbidity associated with the index injuries8,10. Anecdotal reports and recent review articles have suggested that regional anesthesia has the potential to improve pain control in disaster settings9,10,19,20,37. However, the published literature on the use of RA in disasters is limited, and to date no randomized controlled trial has evaluated the efficacy, safety and acceptability of nerve blocks in a disaster context. The planned RAPID study will address these specific gaps in the research21. A key step in executing the trial is appropriately training personnel to carry out the procedures and protocols. This study provides evidence of success in personnel training for a small cohort of generalist humanitarian responders to perform RA.
Standardized assessment and training in research procedures is important in reducing error and deriving valid trial results38. The present study used rigorous methodologies that integrated both interactive didactic sessions and multimodal simulation to train providers in focused RA. The employed training principles are similar to prior documented works in procedural skills and RA training that have utilized systematic assessments of technical skills39,40. Additionally, the assessment methods for technical competency in evaluating procedural abilities were checklist-based, which have been shown to result in more thorough and objective assessments of component skills in multi-step medical procedures41,42. Furthermore, the assessment outcomes for procedural performance, evaluated by independent raters, overall demonstrated excellent agreement, supporting validity in the results31,43. These findings, in conjunction with the significant improvement in interval didactic assessment scores in both the full cohort and individual professional sub-groups, support the efficacy of the training methodology.
Although prior studies have assessed the performance of femoral never blockades after brief trainings in emergency department settings among physician and nurse trainees this study is the first to evaluate formal training of generalist humanitarian response providers in RA methods24,25,44,45. In addition, a prehospital study of pain management for lower extremity injuries performed by emergency medical service providers found that approximately 89% of patients had effective analgesic treatment with provision of prehospital RA26. This prehospital efficacy was replicated in a cohort of paramedic proceduralists employing fascia iliaca compartment blocks in a controlled trial among patients with femur fractures27. The congruent findings in successful RA techniques between the prehospital and hospital based studies and the present work supports validity in the findings and bolsters the feasibility of pre-training generalist providers to perform RA in an acute disaster setting.
This work must be interpreted in the context of certain limitations. The presented results illustrate short-term acquisition of knowledge and skills among the MSF volunteers trained, but do not allow for assessment of application in actual disaster situations, nor for evaluation of skill retention over time. It is likely that similar to most technical skill sets, the study proceduralists will require refresher training prior to execution of the RAPID study, which has been built into the trial design. Although the population of humanitarian responders was drawn from a large pool of MSF volunteer personnel, the cohort was relatively small and not randomly selected, and as such the generalizability of these outcomes to the greater population of disaster healthcare personnel is not certain. During completion of the RAPID study this will be partially addressed, as there will be further onsite training for locally recruited healthcare providers, who will also serve as proceduralists during the later study phases. These later phase providers will be trained and assessed onsite using the same methods as described in this report.
Prior to conducting a trial of RA in a disaster setting, providers need to gain the knowledge and skills necessary to perform the interventions. This study demonstrated high knowledge and technical skills scores with excellent inter-rater agreement between independent evaluators, illustrating the success of the focused training for generalist humanitarian response providers in the selected RA techniques. This work, in conjunction with the planned RAPID study, will contribute to the development of an enhanced evidence base to guide future care and improve health outcomes among high-risk patients injured in the settings of humanitarian emergencies.
Data Availability Statement
The data used for this analysis can be accessed via: https://figshare.com/s/1825267cbf21863b6cf4.
Competing Interests
All authors declare that they have no competing interests to disclose.
Corresponding Author
Adam R. Aluisio, MD, MSc
Warren Alpert School of Medicine, Brown University, Department of Emergency Medicine
55 Claverick Street, Room 274
Providence, Rhode Island 02912, USA
Email: [email protected]
Appendices: Abbreviations
CRED: Centre for Research on the Epidemiology of Disasters
FICB: Fascia iliaca compartment block
FNB: Femoral nerve block
IQR: Interquartile Range
IRR: Inter-rater reliability
LG: Landmark guided
LGFICB: Landmark guided fascia iliaca compartment block
LMIC: low- and middle-income countries
MoH: Ministry of Health
MSF: Médecins Sans Frontières
RA: Regional anesthesia
RCT: Randomized Controlled Trial
SAE: Serious Adverse Events
SD: Standard Deviation
US: Ultrasound
USG: Ultrasound guided
USGFNB: Ultrasound guided femoral nerve block
WHO: World Health Organization
Introduction
Dust storms, which is wind carrying suspended loose sand from a dry surface, are common in arid and semi-arid areas like Iran but rare in Tehran, and planning is needed in order to be prepared for such disasters 1.On June 2, 2014 a sandstorm hit Tehran, the capital city of Iran at 17:15 which was a rush hour in the afternoon when people were heading home. This 110 kilometer (70-mile) per hour wind, which lasted more than 15 minutes, disrupted many functions of the city 2,3. In 1997 in eastern Mediterranean and also 2004 in China, similar incidents with sudden change in the air mass occurred. After the eastern Mediterranean dust storm they found that employing a synoptic network would make it feasible to forecast dust events up to three days before its progression to a significant one 4,5. Xueqin Liu et al, in their study found that in incidents such as extremely severe dust storms which occurred in the Alashan League in the spring of 1993, losses reached an unacceptable level. They declared that economic and other losses might be prevented by planning on disaster prevention, monitoring, and early warning system 6.
Establishing early warning system (EWS) is one of the main parts of disaster response planning which includes four elements: 1- hazard identification, 2-hazard monitoring, 3-sending alert to the risk prone population, and 4-building response capacity 7. This report focuses mostly on sending alerts and enhancing response capacity to present the most important lessons learned at Tehran dust storm in 2014.
Method
Data for this report were collected through Tehran emergency operations center reports and documents, interview with the manager of Tehran Emergency Management Center and from news websites. It was backed up with literature review through “PubMed” with the following key word: “dust storm” and “early warning”.
Results
This incident had a death toll of five (two persons because of falling from buildings, two persons due to falling objects and one is unknown) and 44 injured, who mostly were surprised by the powerful winds. Other impacts were knocked down trees, floating debris, car crashes due to low visibility, temporary power outages, affected Internet and telephone services, delayed flights, and damaged buildings 3. Local news agencies notified that the head of meteorological organization had warned the disaster management organization of Tehran municipality a few minutes before the storm reached the capital city. News agencies also claimed that shortly before the incident, forecasters on the state television initially warned citizens of Tehran to stay indoors, while outdoor people were much at risk. In this incident, the alarm was not transferred to at risk populations and the related organizations in time and in the right manner. Additionally, no safety measures regarding this type of incident had been taught to the people to be taken after the alert had been received.
Discussion
Although the possibility of prediction of such incidents is challenging and needs high technological infrastructure, warning other related organizations after the formation of storm might have been possible 8.
Despite being a rare incident in Tehran, dust storms are common in Iran 9. Therefore, the lesson learned is that for such rare high impact incidents which have short warning time, response planning should focus much more on establishing EWS to give timely alert to the risk prone population. For example, to cover all target population including those staying outdoors, preplanned instruments such as sirens are needed along with routine media broadcasting.
Finally, public education for taking safety measures after receiving the alert or when exposed to the disastrous situation, is recommended towards developing a community-based disaster response.
Competing Interests
The authors have declared that no competing interests exist.
Correspondence
Ali Ardalan MD, PhD. Tehran University of Medical Sciences. Harvard Humanitarian Initiative. Email: [email protected]
Brief Incident Report
On 9 April 2013 at 11:52 UTC (16:22 local time), a Mw 6.2 earthquake occurred at the depth of 20 Km in Dashti district in south-west Iran’s Bushehr province 1. The macroseismic epicenter was located near the city of Shonbeh. The earthquake caused 37 deaths and 850 injuries. Over 1,000 houses in 92 villages were damaged. The earthquake resulted from thrust faulting on a NW-SE trending fault plane, consistent with continuing shortening of the Arabian Plate 2.
According to the International Institute of Earthquake Engineering and Seismology based in Tehran, during one month following the earthquake, a total of 282 aftershocks hit the epicentral region 1. The aftershocks occurred mostly at the east and north of the epicenter 3 and ranged from 2.5 to 5.7 on the Richter scale (RS). The distribution of aftershocks is representative for principal stress direction (NE-SW).
Distribution of aftershocks’ magnitude on the RS was as follow: 33 M<3.0 (11.7%), 171 M3.0-3.9 (60.6%), 70 M4.0-4.9 (24.9%) and 8 M5.0-5.7 (2.8%). Among the 78 aftershocks with M ≥4.0, four aftershocks (5.2%) occurred at the depth of ≤10 Km, 63 (80.8%) at the depth of 11-39 Km, seven (8.9%) at the depth of 40-50 Km, three (3.9%) at the depth of 50-100 Km and one aftershock (1.2%) at the depth of 102 Km 1. Figure 1 illustrates the aftershocks geographical distribution and figure 2 shows a decreasing trend of the aftershocks in terms of number and magnitude over 30 days after the main shock.
(Source: International Institute of Earthquake Engineering and Seismology)
Fig. 1: Geographical distribution of aftershocks following 9 April 2013 Bushehr earthquake
(Source: International Institute of Earthquake Engineering and Seismology)
Fig. 2: Number of aftershocks within 30 days of 9 April 2013 Bushehr earthquake by magnitude on the Richter scale
By definition, aftershocks are earthquakes that follow the largest shock of an earthquake sequence 4. They are smaller than the main shock in size and occur as the touching edges of two plates need to adjust to new positions. This adjustment may takes weeks, months, or years. The location of the aftershocks, however, is not predictable. But, as a general rule, they occur within a characteristic distance from the main shock that is usually taken to be one or two times the length of the rupture associated with the main shock 5.
The aftershocks are potentially able to do additional damage 6. While, any felt aftershock may cause additional damage or create new falling hazards, the risk is higher with those of magnitude 5.0 and larger. The damage, of course, also depends on the site conditions, building type, and distance from the aftershock. This risk is highest for previously damaged buildings 5. Among the aftershocks’ impacts, we remember the collapse of a hotel that caused 44 deaths following the Van earthquake of 23 October 2011 7. A magnitude 5.8 earthquake on 29 May 2012 in Italy is another example. It hit the epicenter region nine days after the main shock and caused an additional 20 deaths and widespread damage, particularly to buildings already weakened by the 20 May earthquake 8.
In Bushehr earthquake, a M5.4 aftershock on 10 April in Chahgah village caused at least four injuries and destruction of several buildings that had been already damaged by the main shock on 9 April, according to the Director of Iran’s National Disaster Management Organization 9. We could not find any other official report or statement regarding the other impacts of the aftershocks in this earthquake.
Lack of a consolidated reporting system on consequences of aftershocks is a challenge as we have also observed in other major earthquakes in Iran, like Bam (2003), Zarand (2005) and Lorestan (2006) earthquakes. This limited our knowledge about the aftershocks induced damages which is necessary for timely risk communication with the affected people and for a long term community education. Because people entering damaged buildings are at risk should an aftershock occur, we believe that this information must be developed and shared with Iranian community to increase their awareness and minimize the risk of further loss of lives.
Competing Interests
The authors have declared that no competing interests exist.
Corresponding Author
Ali Ardalan MD, PhD. Tehran University of Medical Sciences. Harvard Humanitarian Initiative. Email: [email protected]
Brief Incident Report
On 15 April 2012 at around 13:00 local time, following a heavy rainfall in Tehran, a break in the channel wall of Kan River caused a flash flood in the Tehran metro tunnels. Consequently, line 4 of the metro went out of operation for about two weeks 1 . The flood was running for 30 hours in the metro system so that three stations were flooded causing damage to four trains and 28 wagons 2. It is estimated that approximately one million m3 of water and debris rushed in the metro tunnels through the break. Although this flash flood caused property damage of about $21 million (at the official exchange rate) to the metro especially its electrical system, fortunately no death and injury ensued 1,2,3,4 .
Quick measures were taken to disconnect electricity and evacuate more than 1,500 passengers and staff from the adjacent stations while simultaneously the water was draining. For a few days, more than 10 thousands m3 of debris and precipitants were removed from the stations and trains. Finally, damaged stations were repaired and got back to the operation in 12 days 3 . It was claimed that 2,500 persons worked every day during the response to this disaster.
Immediate disconnection of the electricity system prevented electrocutions. Timely emergency evacuation in this event saved hundreds of lives. All trains were stopped in adjacent stations and the passengers were instructed by the staff to safely evacuate the metro. In addition, dwellers near at risk stations were relocated to safe buildings.
Here, we wish to address some challenges along with corresponding lessons learned that have a bearing on revisions to the emergency plan of Tehran in general and Tehran’s metro in particular:
Funding Statement
The authors received no fund for this study.
Competing Interests
The authors have declared that no competing interests exist.
Corresponding Author
Ali Ardalan MD, PhD. Tehran University of Medical Sciences. Harvard Humanitarian Initiative. Email: [email protected]
Brief Incident Report
Less than a year after devastating twin earthquakes in northwestern Iran, an earthquake of 6.1 magnitude hit southwestern Iran near the city of Khvormuj and the towns of Kaki and Shonbeh in Bushehr province on 9 April 2013.123 Being felt in Persian Gulf coast, Qatar, Bahrain, UAE, and eastern Saudi Arabia, the quake was so massive that led to destruction of three thousand houses, 37 deaths (mostly in the town of Shonbeh and its villages) and more than a thousand casualties.4 Thanks to the previous experiences from the 2012 twin earthquakes, the official disaster mitigation committee took immediate actions to coordinate rescue operations.56 Continuous efforts were channeled into searching for the rubbled victims; however, two villages in the Khvormuj district were almost flattened. People rushing from the neighboring areas to offer their help slowed down the rescue process, a similar obstacle faced in 2012 twin earthquakes.7 Overall, 160 victims were transferred to and treated in the Khvormuj hospital, a university-affiliated hospital in Khvormuj district that provided abundant medical services obviating any field hospitals establishment. Nevertheless, 139 survivors were transferred to the hospitals in Bushehr for specialized care. Telecommunication was hampered within the early hours after the earthquake resulting in discoordination among the rescue teams. The similar concern was reported in the 2012 earthquakes in northwestern Iran.58 Except for an emergency need for blood supply which was later met by the neighboring provinces, no serious medical shortage was reported. Unlike the previous experiences in 2012 earthquakes, the number of the fatal casualties was minimal which might have been due to the sufficient 24-hour medical air assistance.5
The survivors have been settled in temporary shelters with adequate primary supplies. Moreover, a psychosocial support team has been sent to the field as the aftershocks are still continuing. However, considering the hot climate of the area, immediate measures should be taken in order to avoid any further casualties particularly heatstroke, dehydration, diarrheal and vector-borne diseases.910111213
Funding Statement
None
Competing Interests
The authors have declared that no competing interests exist.
Correspondence
Dr. Samad EJ Golzari. Email: [email protected]