Methods: The full systematic review applied standard systematic review methodology that was described in detail, peer-reviewed, and published before the research was conducted.
Results: While the science of humanitarian practice is still developing, a systematic review of targeting vulnerable populations in urban humanitarian crises shed some light on the evidence base to guide policy and practice. This systematic review, referenced and available online, led to further findings that did not meet the pre-defined inclusion and exclusion criteria for evidence set out in the full review but that the authors, in their expert opinion, believe provide valuable insight nonetheless given their recurrence.
Discussion: These additional findings that did not meet criteria for evidence and formal inclusion in the full manuscript, but deemed valuable by the subject expert authors, are discussed in this commentary
]]>Introduction
This discussion compliments a full systematic review by the authors published by Oxfam on targeting in urban humanitarian crises: What practices are used to identify and prioritize vulnerable populations affected by urban humanitarian emergencies? A systematic review. Oxford: Oxfam GB.1 Given the rapid growth of cities that outpace public services and extreme poverty marks some, sometimes large, portions of these cities. Even before a crisis, many urban dwellers may live below the Sphere minimum standards and needs can often outstrip the resources that humanitarian aid can bring to bear for disaster affected and non-affected persons in these cities. Identifying the most in need to prioritize for aid can be difficult. The goal of the systematic review was to evaluate the evidence base on targeting vulnerable populations in urban humanitarian crises. Urban vulnerability translates into multiple specific needs and a wide range of need assessment tools and methodologies were reviewed as long as they had been used in an urban humanitarian emergency and its performance had been evaluated. The evidence base was thin but some concrete findings could be drawn to guide practice.
In addition to the studies and findings reported in the full review, we identified 16 reports that were relevant to the topic of the review by meeting criteria for initial screening, but fell short of meeting the criteria for inclusion in the formal evidence-based synthesis. The predefined inclusion criteria for inclusion in the systematic review required that reports a) described a targeting practice had been employed in an urban humanitarian crisis and; b) that the practice was evaluated in some form or another. Standard systematic review methodology was used and a protocol for the systematic review was reviewed and published prior to the research. For the detailed methodology used in the systematic review including key terms of reference please refer to the original publication. As expert authors, we believe repeated lessons within these 16 reports provide valuable insights, reinforce the full systematic review findings or represent promising areas of research for further study despite their lack of supporting evidence as defined by the full systematic review methodology. This editorial commentary on targeting was focused around these recurrent lessons identified through the same thematic analysis used in the full systematic review. These summary commentary lessons from the full systematic review and these additional 16 reports about targeting approaches and other features of targeting are summarized in Table 1 and Table 2, respectively. These tables aim to provide a full accounting of our expert recommendations in an easily digestible format and represent a current ‘state of the art’ reflection of the our guidance on targeting practices for vulnerable populations in urban crises.
Given the overall lack of study, we argue that the absence of evidence does not necessarily make these lessons untrue. In fact, their repeated nature would actually qualify them as valid findings according to other criteria and they may eventually be supported by evidence. We included examples from the 16 reports within the commentary to provide a clearer depiction of the content discussed, not as anecdotal evidence.
Commentary from Recurrent Lessons
Targeting ‘Affected’ vs. ‘Non-Affected’ populations does not work well
In addition to targeting by displacement status, as highlighted in the full systematic review, targeting only persons affected by a crisis, those experiencing some loss as a result of the crisis, does not generally work well in the urban space even when resources are limited. Targeting only persons directly affected by the crisis such as those that suffer material or bodily harm directly by the crisis does not identify all or even the most vulnerable in urban humanitarian emergencies.2 To begin with, delineating who is ‘affected’ is difficult. Urban areas are complex systems in which a humanitarian emergency can have many indirect impacts on the ability to keep safe and obtain necessary goods and services making it difficult to truly define ‘affected or ‘non-affected.’ A flood may cause food prices to spike or foment violence that impacts households not directly damaged by floods themselves. Defining ‘affected’ is a critical challenge in this strategy. Additionally, chronically high levels of vulnerability within urban environments, sometimes themselves classified as (or otherwise meeting the criteria of) humanitarian crises, result in increased levels of baseline vulnerability among host or pre-crisis populations.3 Even after a crisis strikes, these poor but ‘non-affected’ populations (however defined), may be as or more vulnerable than persons that are directly or indirectly affected. The needs and vulnerability of ‘unaffected’ urban populations, especially the urban poor, may fall well within humanitarian imperatives and the goals of the targeting program. Targeting by ‘disaster affected persons does not work well in urban areas to accurately identify all or the most persons in need of a specific humanitarian aid interventions services.
Targeting upstream individuals and groups can enable recovery for the most vulnerable
Focusing on employers or individuals who are responsible for the livelihoods of others can be a means of returning beneficiaries to baseline livelihoods more quickly.4 In their review of cash transfer programming across a variety of settings, IIED highlighted the importance of keeping in mind that the most-affected populations, and those vital to post-crisis recovery, may actually be the relatively better off, such as small business owners who employ lower income individuals.5
After the January 2010 earthquake in Haiti, targeting in one program focused on small business owners in an effort to help businesses remain in operation. Targeting focused on both the low-income as well as the middle-income groups “for two reasons: first, the middle groups were also badly affected by the earthquake and secondly, the services and activities carried out by the middle groups play a vital role in the recovery [of] the economy.”6 Focus groups in Haiti identified many vulnerable groups who were in need but who had not been targeted to receive services, including teachers. These focus groups identified the key link teachers provided in maintaining the human resources necessary for the education system and concluded that teachers should be prioritized as beneficiaries.7Incorporating this form of upstream targeting can facilitate smooth exit strategies and shifts the focus of targeting to engaging local actors.
Poverty is a useful but imperfect proxy for vulnerability when used alone
Targeting vulnerability more generally based on poverty alone as a proxy may be appropriate in urban settings but requires detailed understanding to target correctly. A snapshot of income or assets alone does not account for an accurate understanding of vulnerability. As identified by MacAuslan and Farhat, poverty measures alone do not account for current or anticipated needs or the impact of a crisis on various socio-economic groups.8 Socio-economic variables including an assessment of coping strategies needs to be incorporated into targeting processes for more accurate targeting. Someone with less poverty may in fact be more vulnerable because they have more to lose or their means of living in the urban area are dependent on certain urban functions that can be impacted by a crisis or they may lack sufficient coping mechanisms. Urban areas constitute an economic environment with goods and services driven by markets and thus poverty is key but does not wholly reflect vulnerability, which is multidimensional.
Protection concern may drive vulnerability more than other measures in some situations
Despite having low vulnerability according to various indicators such as income or displacement status, concerns about safety may actually drive vulnerability in some cases. These protection concerns may override many other indicators of vulnerability.9 Protection concerns, however, may be linked to one of these specific indicators such as status as a refugee, residence within a conflict zone or engagement in child labour. For example, although a household may enjoy a higher socioeconomic status, female heads of household or specific ethnic groups may actually have limited access to basic goods and services due to constrained mobility from insecurity and fear of violence in the urban space. Targeting approaches should add a protection lens to vulnerability analyses keeping in mind that safety and security can be paramount to wellbeing.10
Geographical targeting requires more detailed analysis given the density and heterogeneity of cities
Geographic selection of urban areas to identify vulnerable populations by specific location, such as slums or low-lying coastal zones, can be a very effective process for targeting.8,11 However, because many urban areas are not homogenous, care should be taken to identify geographic units that are smaller and not restricted to typical municipal or administrative boundaries.5,9,12 Vulnerability is heterogeneous and ignorant of such boundaries in urban areas.
Community participation and community based targeting are key to effective response but must be used with caution
Many of the reports point toward the importance of community perspectives to help ensure that vulnerable areas and populations are not overlooked.5,8,9,13 Incorporating community perspectives can lead to locally derived measures of vulnerability as described in the full systematic review. Such locally derived measures, however, take time and resources to develop. They may often lose comparability between contexts depending on their design. Yet comparable tools can be developed. For example, a scale based on local coping strategies can allow comparison if variations of coping can be applied to the same quantitative scale. These trade-offs must factor into their selection.
Community based targeting (CBT) or participatory targeting whereby the community directly identifies vulnerable persons or households is a growing practice in humanitarian interventions and compliments trends toward locally driven processes that are inclusive and suited for area based programming. The data from these practices is thin and of low quality but common lessons are repeated. In general, incorporating community knowledge is clearly vital to good targeting, but participation can take many forms.
Lessons indicate the importance of having a nuanced understanding of the motivating factors driving individual participation in community-based targeting, as well as familiarity with local power dynamics and knowing whose voices are being heard.4,14 As such, defining the community is critical and must be done carefully. Reports suggest that, in many ways, the community-based targeting practices relied upon in rural areas may not be relevant in urban contexts. Two reports highlighted the greater risk of using CBT in urban areas because close geographic proximity in urban environments may not necessarily indicate familiarity within communities as much as it may in rural areas, due to population mobility and fractured social networks.5,15 As a result, CBT that relies too heavily on community leaders or a small subset of people to identify beneficiaries can lead to biases and systematic exclusion of vulnerable groups or individuals more than in rural areas.5,15 Maintaining accuracy with community-based targeting requires triangulation and verification of information, as the most vulnerable neighbors may be unknown to or marginalized by community leaders.16Community engagement that unwittingly reinforces any pre-existing marginalization will do more harm than good.
Measuring food security an take many diverse forms but requires detailed analysis
Papers on targeting for food insecurity were more numerous than other forms of sector-specific targeting, with 10 of the 21 evidence-based articles in the full systematic review dealing specifically with food security. Indeed, many of the evidence-based lessons and recurrent lessons above came from food security reports yet applied more generally as well. There was a lack of evidence directly comparing measures but a few insights are found in the various reports.
Targeting for food aid can measure a variety of characteristics such as consumption, purchasing power, access, nutritional status or coping strategies. These measures take multiple forms from a universal composite index to a locally derived context specific scale. All of these approaches come with their own advantages and disadvantages.17 Measuring nutritional intake or status provides only a snapshot of current or past consumption patterns. It does not accurately reflect food security, which is a latent property representing the ability to secure adequate food. Several other methods such as the Household Food Insecurity Assessment Scale attempt to do just that.18 By identifying a few key indicators, assessments may rapidly and efficiently identify vulnerable households and optimize targeting without extensive data. Although food prices play a large role in food consumption in urban areas, poverty alone is not always the best correlate for food insecurity. To identify food insecure populations, understanding intra-household consumption patterns, capturing out of home consumption and the local coping strategies employed in additon to standard tools is key.
Involving local markets is important to targeting in urban areas while enhancing overall recovery
Markets are important to addressing vulnerability in urban areas. Multiple reports point toward the importance of market analysis as urban food security is closely linked to commodity prices, income opportunities and wage rates.19 One key insight from Oxfam programming after the 2010 earthquake in Haiti was that “a better understanding of crucial market chains can help lead to a more effective distribution of humanitarian resources, faster economic recovery and less risk of long term dependency on external assistance.” The program in Haiti relied upon an inter-agency Emergency Market Mapping Analysis (EMMA) as well as a 2009 baseline assessment of income groups within Port Au Prince to create wealth group profiles for households affected by the earthquake and to inform targeting.6
Programming aimed at improving market recovery post-crisis can also achieve the dual purpose of improving livelihoods as well as nutrition. The review uncovered several studies that provide specific examples of how effective targeting involving local markets improved livelihoods. In Bulawayo, Zimbabwe, a program aimed at improving the nutritional status of vulnerable households successfully used local millers to produce, and existing retailers to sell, a low-cost maize alternative—sorghum.20 Oxfam used cash transfers in Nairobi to help households meet food needs through local markets and found that, along with other services to support entrepreneurship, the program enabled 50 per cent of beneficiary households to initiate, strengthen or restart a small business, creating more vibrant local markets.21 Additionally, an evaluation of the canteen program in Haiti after the 2010 earthquake found that 87% of beneficiaries who received small business grants were able to restart an economic activity and 64% of the women participants were able to restart their business because of the canteen program.6
Vulnerability can be invisible
It is important to acknowledge that the most vulnerable persons may be those who try to stay invisible to authorities and even their neighbors, and therefore may be missed by the targeting methods discussed in this review.4 This need for anonymity makes them particularly vulnerable. Also, a lack of representative leadership structures among refugee communities may result in individuals being overlooked or invisible to members of their own community.22 One proposed solution is to provide discreet community drop-in centres open to all that allow invisible persons to self-target for protection or service provision.22 Another proposed solution to connect with beneficiaries is to publicize hotlines where beneficiaries can call and receive information about services.23 All of the proposed solutions for this population require focused study.
Table 1: Targeting strategies, review findings and other notable advantages and disadvantages to guide selection.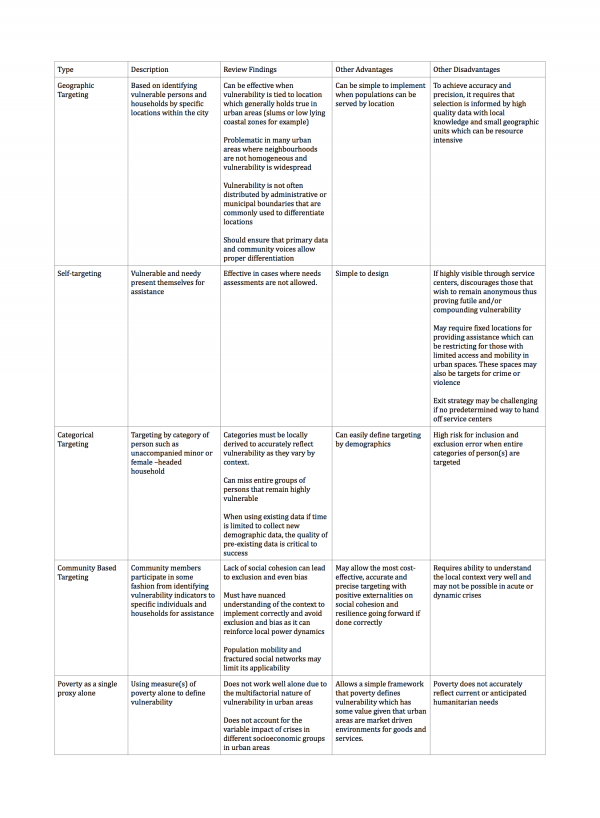
Table 2: Other features of targeting, review findings and notable advantages and disadvantages to guide selection.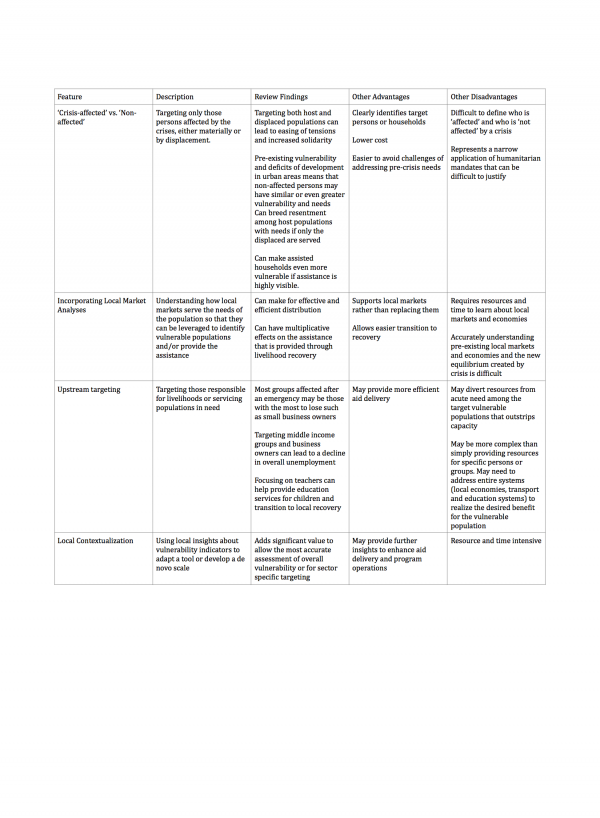
Conclusions and Recommendations
The current evidence and recurrent lessons above do not point to one single best approach for targeting vulnerable populations in urban crises. As humanitarian programs have a wide variety of goals and urban contexts and crises vary, the complex nature of vulnerability makes it impossible to have one best approach for each situation. Any approach will have strengths and limitations and none will be perfect as needs may often exceed available resources. In addition to these technical limitations, the security situation and political context can also impact the selection of a targeting approach. While evidence to guide humanitarian practice accumulates further debates on the humanitarian system and financing will have to progress in ways that incentivize evidence based practice. Selection of targeting vulnerable populations in urban crises will have to weight the costs, benefits and feasibility of each approach and funding tied to evidence on how these three variables are assessed will be the best path moving forward.
Vulnerability in urban areas is complex and interconnected such that assessing sector-specific vulnerability seems inappropriate or at least less useful. A person’s health and nutrition for instance is related to their shelter, access to sanitation, livelihood and surrounding security. We believe the most vulnerable in urban humanitarian crises are best targeted using a collection of socioeconomic indicators along with in depth contextual understanding.
Given that local actors, including government, will play a larger role in humanitarian response and the knowledge that municipal authorities and pre-existing organizations have, leveraging pre-existing data will be valuable. Often these may be incomplete, outdated or biased but improving these sources of information beforehand could be prove useful and efficient. As development and humanitarian practice come closer together within a resilience framework, reducing urban vulnerability as part of development efforts could help inform targeting in the event of a humanitarian crisis. Practices for targeting vulnerable populations in urban crises should leverage urban development practice and tools in rapidly growing cities that aim to alleviate poverty and build resilience.
Additionally, as the local expertise of already established actors and the affected community itself can prove invaluable, community based targeting (CBT) should be developed and tested further. The success of such an approach will depend on local capacity and technical expertise. Entrenched biases and power-dynamics may also bend a very well-intentioned approach into exacerbating vulnerability and a nuanced understanding of this context is required. The recent focus on area-based programming leans toward using a CBT approach as a key component. Targeting approaches should exploit local knowledge and community based approaches with a nuanced understanding of these communities and power relations.
Finally, the most promising approach may in fact be targeting based on methods that can be locally contextualized and rapidly so given the important of balancing accuracy with speedily delivering aid. As spaces within cities can be micro-environments that differ from neighbourhood to neighbourhood, locally contextualized tools should be further developed and expanded. Research and practice should focus on developing and testing rapidly tools that can be quickly contextualized to the local situation.
Overall, the full systematic review and this commentary from recurrent lessons lay bare the general lack of evidence guiding practice in targeting the most vulnerable in urban crises. Focused research and funding for it, as discussed in the full systematic review, must be prioritized to ensure humanitarian practice is grounded in rigorous evidence.
Corresponding Author
Ronak B. Patel, [email protected]
Data Availability
All relevant data are included within the paper.
Competing Interests
The authors declare the following interest: DS serves on the Editorial Board for PLOS Currents: Disasters. He has not influenced or played any role in the peer-review, editorial decision making or publication of the manuscript.
Article
In 2004 I was honored to be interviewed for the Lancet medical journal’s Lifeline Series.1 I had just come away from a disastrous short tenure as the Interim Minister of Health in Iraq following the 2003 war. I had support from former Secretary of State Colin Powell to rapidly mitigate and recover the war related destruction of essential public health infrastructure and protections required as Occupiers under Articles 55 and 56 of the Geneva Convention (GC) that follow every war. Predictably, the loss of essential public health protections in food, water, sanitation, shelter, health, and energy leads to excess and preventable mortality and morbidity, numbers that exceed those from war weaponry by 50-70% or more.2 This plan was immediately squelched by an unprecedented decision within the Bush Administration that moved these post-hostilities humanitarian responsibilities from the State Department to the Department of Defense under Donald Rumsfeld. This decision claimed that US forces were not ‘occupiers’ but ‘liberators’, promptly reversing any previously planned public health recovery and rehabilitation. The State Department’s coterie of seasoned nation-building experts, including myself, was summarily replaced. Before leaving Iraq I publicly declared Baghdad a public health emergency but this too fell on operational deaf ears.3 Many in Iraq see that decision as the most egregious of policies enacted after the invasion, in which the elderly, children, woman and disabled primarily suffered the most. While the ‘liberator’ claim was debunked and reversed 18 months later, it was too late. Without a reliable public health data and surveillance system, also thwarted in the war’s aftermath, the political powers remained protected from further scrutiny. Thirteen years later, Iraq remains a public health emergency.4
The Lifeline interview asked several questions: “What did I believe was the most exciting field of science?” My answer: “Public health. It has the most potential and the least support.” The interviewer, surprised, stated that to date no one had ever mentioned public health. When asked what I thought was the greatest political danger to the medical profession I answered: “Political interference in public health.”1
My answer today would be the same. We continue to see how the decades old international legal framework is easily overwhelmed by political inaction, interference and moreover, struggles for relevance given today’s modern challenges. The reasons for humanitarian crises and how the world must respond to them have dramatically changed every decade.5 The 1945 United Nations (UN) Charter, International Humanitarian Law (IHL) and the 1949 GC was designed to protect humanitarian aid in cross border wars. Unfortunately, while the language remains relevant and attempts have been made to adapt to modern day intrastate wars, too few warring factions and signatory governments either respect, or are unwilling, incapable, or selectively and blatantly ignore the protections we in the humanitarian community found sacred. No longer is their assurance for the continued safety of citizens, military casualties ’out of combat’, vital public health infrastructure and protections, and humanitarian personnel in intrastate unconventional armed conflicts. As political oppression and armed conflict erupts, essential public health infrastructure rapidly disappears and populations flee. If one accepts that disasters keep us honest by defining the public health and exposing its vulnerabilities, the global community must emphasize prevention and preparedness and re-legitimize it under international law to ensure protective strategies that intercede in fragile states before they deteriorate to the point of no return.
More than a decade after the Iraq war, a broader brand of global health engagement has emerged yet public health’s role within that rubric remains in limbo, is operationally ignored, or is ill defined. What sanctioned interventions exist ‘under international law’ to protect the public health before conditions deteriorate? None are clearly defined. Working from existing laws of war, the ICRC, influenced by the consequences of Iraq and now Syria, acknowledge the overwhelming and dramatic “cumulative impact that stems from the complexity of urban system” collapse and their mutual dependence on country-wide large-scale inter-connected infrastructure loss that the health systems are not able to keep up with.6 The numbers killed or injured are unprecedented. While today we painstakingly attempt to document the loss of health personnel in war, there is no equal documentation of essential public health recovery personnel, especially in water and sanitation.6 Despite the desperate call for a renewed emphasis on disaster risk reduction in 2015’s Hyogo Framework for Action, the fledgling global community is fixed on interventions that still favor response over preparedness and prevention for natural disasters. But what if the consequences of a natural disaster, including that of climate change, are inextricably leading to conflict or war?
Today’s domestic and regional crises are increasingly under the influence of widely integrated global changes and forces defined by climate change, biodiversity loss, emergencies of water, food and energy scarcity and rapid unsustainable urbanization. These crises, initially slow moving, are increasingly severe affecting massive populations across many borders. Drought, crop destruction, and famine coincide with loss of vital aquifers. Whatever limited and often primitive public health protections remain, they have proved ineffectual, dangerously managed and selectively denied to the most vulnerable by those in power who persistently ignore wide ranging mitigation advances offered by the scientific community.
New legal preventive protocols and epidemiologic surveillance approaches are needed to protect civilians. Protecting the public health must be viewed both as a strategic and security issue requiring close collaboration with humanitarian, and military logistical and security personnel. Any attempt to redefine public health as a security issue must be coupled with efforts to develop a more comprehensive accounting of the human cost of modern-day fragile and ungoverned territories—not just warfare.
A mandate for a universally accepted system of preventive monitoring of more precise methods and outcome indicators that measure the effectiveness and efficiency of national health and public health systems is undeniable. However, health alone cannot solve these global health problems. While some standard indicators are already available, the most sensitive are often multi-and trans-disciplinary. For example, rates of dengue fever, which escalate when trash collection is inadequate, are sensitive indicators for economists of both poor governance and urban decay.7 The humanitarian community is far from realizing this goal. For instance, we do not know how to operate effectively in unsustained dense rapidly urbanized settlements, a most likely site of future major conflicts. Unless measures are taken to develop ways to include indirect mortality and morbidity, calculating the human cost of public health decline will remain an inexact process of estimation by political scientists, humanitarians and military analysts. Capacity to access vital information of the location, function and extent of destroyed essential infrastructure is currently “not accessible.”8 The lives at risk and those lost will remain unseen, uncounted and unnoticed—and the lessons for effective prevention and protections unlearned.
Crises only gain international attention when they result in conflict. The Syrian conflict is a case in point. From 2011 to 2016, 60% of Syria’s agricultural northeast and south suffered its worst drought, water shortage and crop failure, compounded by failures in governance and management. Poverty accelerated the exodus of farmers, herders and rural families to cities in the west fomenting today’s major sectarian war. Multiple public health interventions were available and could have ceased or mitigated the decline and population exodus.9 Similar lost opportunities for preventive engagement occurred in the Sudan, Somalia, Eritrea and Ethiopia.
Indeed, if all the forcibly displaced persons would be placed in one state it would be the 21st largest populated country in the world.10 Populations escaping from public health collapse—as internally displaced or refugees—will exceed those from warfare alone, further adversely affecting the fragile public health protections in host countries such as Jordan, Lebanon, Turkey, and Greece. The humanitarian community, strongly adhering to the global political commitment of ‘responsibility to protect’ endorsed by all member states of the UN must also recognize that migrants have an equal right to live and thrive in the country and culture in which they were raised.11 Not surprisingly, many migrants to the EU have openly declared their dream to return to their native country.
UN sanctioned revisions and rewrites of the IHL and the GC are crucial. The ICRC reports that there is “still room to strengthen and clarify the existing legal framework” to “adapt to new realities”; and, talks of supplemented GC Commentaries that “will give state and non-state actors an understanding of the law as it is widely interpreted today so that it is widely applied effectively in modern armed conflicts.”12
More than ever, we need strong international humanitarian laws and an effective accountability and recourse mandate for those who fail to respect the laws that are in place. Why wait for conflicts to occur when we have a clear evidence-based global mandate to mitigate the obvious public health consequences? With public health infrastructure and protections “absent, destroyed, overwhelmed, not recovered or maintained, or denied to populations” it has become a massive global health emergency.13
While we have had ‘laws of war’ for centuries, is it time, in an increasingly globalized world plagued by public health emergencies, for laws of prevention? Public health protections are a human right. What can one hopefully say to an emerging global society’s credibility that it has the tools to wage war but not to prevent them? The scientific expertise exists to be a force in preparedness and prevention; the political will and international law mandates must follow.
Competing Interests
The opinions expressed in this article are the author’s own and do not reflect the view of their affiliated institutions.
Corresponding Author
Frederick M. Burkle, Jr.: [email protected]
Introduction
The 10th annual Philippine National Health Research System (PNHRS) Week Celebration, from the 8th to 12th August 2016 in Puerto Princesa, Palawan, Philippines, brought together health researchers, policy makers and practitioners from across the Philippines. The conference theme Research and Innovation for Health and the Environment aimed to facilitate smoother exchange of health-related research among key stakeholders via ten pre-conference events, seven parallel sessions, and two plenary sessions. This year’s conference saw an unprecedented focus on Disaster Risk Reduction (DRR). The purpose of this publication is to formally document and communicate the key messages that emerged from the conference.
The 10th PNHRS Week Celebration placed the Sendai Framework for Disaster Risk Reduction (Sendai Framework) at the front and centre of its agenda, highlighting the growing recognition among researchers and policy makers of the need to bolster research in this area within the Philippines. The key DRR-focused events included the Pre-forum workshop on Framework for Disaster Research in Health, the parallel session National Health Research Program on Disaster Risk Reduction and the plenary session on The Philippines as a Research Hub on Global Health Innovations to Deal with Climate Change and Natural Disasters. These events highlighted key strengths and challenges of DRR research in the Philippines within the broader context of positioning the Philippines as a global hub for research and innovation in DRR.
The year 2015 has been noted as a historic year in international policy, with the finalisation of three landmark United Nations agreements. These are:
Further to these agreements, the Sendai Framework was followed by the UNISDR Science and Technology Conference on the Implementation of the Sendai Framework for Disaster Risk Reduction 2015–2030 in January 2016 which included in its recommendations the ‘Need for formal ‘‘national DRR science-policy councils/platforms’’ or a form of national focal points for science to support disaster risk reduction and management plans identified’ 3. A second conference on the implementation of the health aspects of the Sendai Framework for Disaster Risk Reduction 2015-20305 in March 2016 lead to the Bangkok Principles which aim to strengthen health implementation of DRR5. Additionally, the landmark paper of the 2015 Lancet Commission on Health and Climate Change, called for health to play a larger role in tackling climate change, viewing climate change as an opportunity and necessary area of strengthened action for the health sector in coming decades 6.
Background to the impact of disasters on the Philippines
Widely recognised as one of the most disaster-prone countries in the Asian Region, and the world 7, the Philippines was ranked second on the World Risk Index in 2014 in terms of exposure and risks to natural hazards 8. The Philippines was also the 5th most affected country by natural hazards from 1994 to 2013, and ranked as the most affected country in 2013 according to the 2015 Global Risk Index9. Between 1993 and 2012, the Philippines experienced 311 extreme weather events, the highest number globally, and falls within the top ten countries in the world most affected by extreme weather7. Most recently, the Philippines was found to have the highest expected annual mortality, affected population, and loss in GDP globally in relation to climatic hazards 10. This data is to the exclusion of impacts associated with non-climatic, biological or technological hazards.
The country is exposed to a variety of hazards across all categories – natural, biological, technological and social hazards such as mass gatherings11. Several geographic factors contribute to the high natural hazard exposure of the Philippines, including the country’s location in the ‘Pacific Ring of Fire’ at the junction of two large tectonic plates, the Philippine Sea Pacific Plates and the Eurasian Plate, facing the Pacific Ocean12 and one of the most active typhoon belts in the world 13.
In addition to these exposure factors, significant vulnerability as a result of inequity in access to healthcare and social protection mechanisms, as well as rapid unplanned urbanisation and development in economic hotspots, contribute greatly to the disaster risks faced by the population and economy of the Philippines 8,14.
DRR in the context of climate change has become a national priority with structures established to address these challenges. The national government has enacted the Climate Change Act of 2009 (RA 9729) and established the Climate Change Commission at the national level 15. The National Disaster Risk Reduction and Management Act of 2010 (DRRM Act, RA. 10121) has also been enacted and corresponding structures established 16. These structures are known as the National Disaster Risk Reduction and Management Council (NDRRMC), and are replicated at regional levels, known as Regional Disaster Risk Reduction and Management Councils (RDRRMC). National frameworks and plans in DRR and climate change have been developed and are in various stages of implementation 17 with the sunset review of the DRRM Act currently underway. Within the Department of Health (DOH), health emergency preparedness and response structures are institutionalised at the national level through the Health Emergency Management Bureau18.
The combination of these three factors, the risk profile, experiences and established structures in DRR, positions the Philippines to potentially become an international leader and global hub for DRR. However, several aspects need strengthening to support the development of the Philippines as an international hub for DRR. The key areas for strengthening identified through analysis of the content presented at the PNHRS Week Celebration include: integrated national hazard assessment, strengthened collaboration, and improved documentation.
Science and technology innovations in the Philippines and areas for further development
In addition to the institutional structures mentioned above, the Philippines has relevant scientific and technical structures to contribute to the understanding of hazards and risks, and development of scientific innovation in DRR. These are coordinated by the Department of Science and Technology (DOST), and include, but are not limited to, the Philippine Institute of Volcanology and Seismology (PHIVOLCS) and the Philippine Atmospheric Geophysical and Astronomical Services Administration (PAGASA), to contribute to the understanding of hazards and risks, and development of scientific innovation in DRR.
Local governments are mandated to mainstream DRR and CCA in their local Comprehensive Land Use Plan (CLUP) and Comprehensive Development Plan (CDP). It is intended that these plans use vulnerability analysis and assessment within an integrated DRR and CCA framework 19,20,21. Further to this, Health Emergency Preparedness and Response and Recovery Plans at a regional and local government level contain natural hazard assessments for their corresponding areas 21. These hazard assessments provide potential sources for contributing to a detailed and integrated all-hazard assessment for the nation.
Examples of recent innovations in hazard mapping and assessment showcased during the PNHRS Week Celebration include the Nationwide Operational Assessment of Hazards, known as ‘Project NOAH’ and ‘FaultFinder’. Both of these web-based applications providing information on various hazards in the country, including meteorological and climatologically hazards, as well as major fault systems and earthquake risk mapping. Using a layered approach to mapping hazards, Project NOAH, allows users to select or search for a location and provides weather updates, data on rainfall and river inundation, as well as real time information on rain, weather and tides. The web-GIS tool provides hazard maps for floods, landslides and storm surge. It provides updates on flood reports, information on jurisdictions and critical infrastructure, as well as an impact assessment in the event of a hazard (available at: https://noah.dost.gov.ph/) 22. FaultFinder maps active fault systems, and allows users to search active fault systems of interest using GPS location on their mobile device, by name of location, and by browsing a detailed map view (available at: https://faultfinder.phivolcs.dost.gov.ph/) 23. These projects aim to advance scientific research and risk communication.
A health-based technological innovation cited by the Department of Health at the PNHRS Week Celebration was ‘Surveillance in Post Extreme Emergencies and Disasters’ (SPEED). Developed through a collaboration between the Philippines Department of Health and the WHO Philippines, SPEED uses web-based software to assist in gathering data relating to communicable and non-communicable diseases and conditions in extreme emergencies and disasters 24. SPEED gathers syndromic information from health facilities such as Evacuation Centers and Barangay Health Stations or Rural Health Units, and initial diagnoses from hospitals and private clinics 24. Data can be entered via manual encoding, SMS, or online. SPEED enables the monitoring of trends and early detection of disease outbreaks with the aim of providing timely and appropriate health response to minimise morbidity and mortality in an emergency or disaster 24.
Challenges in collaboration on DRR research in health was a key challenge noted by PNHRS conference participants. A key barrier to collaboration, which was noted by participants during the event, was the lack of awareness and documentation of DRR research and activities. Further to this, it was observed that there was limited representation of other government sectors, UN agencies, private sector and NGOs present at the event. Strengthened documentation of DRR activities, as well as involvement of these stakeholders in relevant future events will help to promote the establishment of the Philippines as a hub for DRR and build full cross-sectoral and cross-stakeholder engagement in the initiative.
Barriers to documentation of DRR research, policies and activities highlighted during the PNHRS Week Celebration include: lack of prioritisation of DRR research and documentation, as well as a lack of system and capacity for documentation. Prioritisation of DRR research is particularly absent in the context of health-related research, with the current National Unified Health Research Agenda for 2011 to 2016 making no direct mention of disaster-related research in health 25. While DRR research in health was acknowledged by panelists to be occurring, this research is happening on a limited scale, and is not included in existing national health research databases.
Two national registries for health–related research were promoted at the PNHRS Week Celebration, including the Health Research and Development Information Network (HERDIN) and the Philippine Health Research Registry. A recent search of these databases reveals limited documentation of DRR research in health and for those that were documented there was limited availability of related publications and outcome documents. At this point there exists no central system for documenting disaster-specific research. Key messages from the DRR sessions at the PNHRS Week Celebration included a need to prioritise and document DRR research if the country which could be developed as an output from possible global hub for DRR.
The conference participants considered that it would be beneficial to strengthen the documentation of DRR research and strategies to build the credibility and evidence base for the Philippines as an international exemplar for DRR and disaster risk management (DRM). To address the challenges in documentation, it would be helpful to consider the need for:
Proposal for the Philippines developing a Global Hub for DRR
Promotion of the Philippines as a global hub for DRR research and innovation to support the implementation of the Sendai Framework has the potential to strengthen DRR investment in the country. The establishment of relevant laws, structures, and technical capability demonstrates the importance of, and existing commitment to, DRR in the Philippines. These factors lend themselves well to this development of the Philippines as a global hub for DRR and DRM.
Experts and policy makers whom attended the PNHRS event frequently referred to the Philippines as a ‘laboratory’ of disasters in Asia. Panelists at the PNHRS identified the importance of climate change and the role of the health and the wider scientific community in developing the scientific and technological capacity of the Philippines in DRR. Within this context, panelists recognised not only the extensive risk profile of the country, but also the significant knowledge and experience developed in DRR and DRM through its established DRR structures.
The concept of developing a national focus in science and technology in the Philippines started more than two years ago as a key outcome of the partnership between the PCHRD and COHRED (the Council on Health Research for Development, accessible via this link: https://www.cohred.org/). Through this partnership the first Global Forum for Research and Innovation for Health in Manila in August 2015, “Forum 2015”, was hosted jointly by COHRED, PCHRD, DOH and DOST 26,27. The ‘hub’ concept intends to create a focus for national development, particularly through inter-departmental and inter-sectoral action, as well as international collaboration 28. Developing a ‘hub’ also aims to optimize the socio-economic impact of investments in science and technology.
Initial interest in the Philippines of becoming a leader in shaping the global research agenda in health and science more broadly was stated at Forum 2015. The event focused on how research and innovation can improve food security and nutrition, health in megacities and, most importantly, DRR. The DRR events that took place during Forum 2015, showcased examples in DRR from several nations, including the experience of the Philippines in strengthening and mobilizing local government units and communities for DRR 27. In the period following Forum 2015, COHRED and PCHRD outlined the field of concentration more sharply in a first concept paper prepared for DOST and DOH: the interface between science and innovation and the impact of disasters – or DRR – with health as a key outcome measure 28. This then became the basis for further internal and external consultations and for making this the focus of the 10th PNHRS Anniversary meeting in Palawan.
At the recent 10th Philippine National Health Research System (PNHRS) Week Celebration, the rationale for developing the Philippines as a hub for DRR was presented and well supported by the panelists from the PNHRS, the Department of Science and Technology, Department of Health and key national and international academic and private sector stakeholders present. During the plenary session, key stakeholders in DRR and health and the wider sciences and private sector demonstrated widespread support for the push to develop the Philippines as a global hub for innovations to deal with climate change and natural disasters, using an all hazard approach. Panelists in the plenary placed health as a central contributor to DRR, particularly recognizing that ‘zero casualty is not zero damage to health’ 29, and the need to reduce hazard exposure and vulnerability, as well as increase coping capacity within the context of health innovations for climate change and disasters 29. Panelists made note of the established structures and human resources that are already committed toward DRR in the Philippines, as well as the desire to share the experiences and expertise of the Philippines in addressing disaster risks 30. With the Sendai Framework providing a method to build research activities and outputs in order to enhance DRR capabilities, the Philippines could position itself as a global hub on DRR 31. However, there is a clear deficit in documentation and publication of these experiences and expertise, which needs to be addressed 32. Panelists also showcased the growing engagement of the private sector in strengthening DRR and clear support for developing the Philippines as a hub for DRR 33. Placing the Philippines at the centre of the converging points on health and the wider sciences addressing sustainable development, DRR and Climate Change Adaptation would be beneficial 34.
The positioning of the Philippines as a global hub could require significant financial investment, however, this has the potential to provide return on investment in DRR 35. An important reference was made to the triple dividend of DRR investment 36, where:
Overwhelming support by key political stakeholders was demonstrated for developing the Philippines into a global hub. This was echoed in the strong rationales presented by panelists in the DRR-related events, as well as by the attendees of the conference. The panelists of the DRR-related sessions clearly presented compelling reasons why the Philippines is well-positioned to become the global hub for DRR. These reasons include the disaster risk profile of the Philippines, experience in DRR and established structures necessary to support the initiative.
Conclusion
As a consequence of its disaster incidence, especially with regards to the frequency and intensity of climate-related extreme events, the Philippines is widely recognised as one of the most at-risk countries in the world, with a developed strength and experience in DRR. This conference demonstrated the emergence of commitment towards using these experiences to strengthen DRR at Barangay, local, regional and national levels. The equal commitment demonstrated towards sharing these outputs with other at-risk countries globally is the driving force behind developing a global hub in the Philippines. The event also highlighted health research as a pivotal area for development in strengthening DRR in the Philippines towards the development of a global hub.
The commitment to the hub was announced at the 10th Philippine National Health Research System Week Celebration. Continuing work to determine what this might mean and how this concept might develop, particularly in the context of science and technology for health in DRR, will be undertaken prior to the presentation at the Global Platform for Disaster Risk Reduction to be held in May 2017 in Cancun, Mexico on 22-26 May. The Global Platform is the premiere international forum dedicated to the international DRR agenda and the 2017 Global Platform will be the first opportunity for initial assessments of the progress towards the Sendai Framework (The Global Platform website can be accessed via this link: https://www.unisdr.org/conferences/2017/globalplatform).
Competing Interests
The authors would like to make it known that Virginia Murray is an editor on the Review Board for PLOS Currents: Disasters.
Corresponding Author
Primary: Banwell, Nicola M.; Email: [email protected]
Secondary: Opeña, Merlita M.; Email: [email protected]
Introduction
Disasters regularly have devastating effects on populations worldwide 1,2. To assist affected countries an increasing number of international emergency medical teams has been deployed 3. Concerns regarding the standard of medical care provided and the lack of preparedness of the teams have been raised. Health practitioners have been observed to work outside their scope of practice and license 4,5, and teams have lacked the basic capacities and means to be fully self-sufficient 2,6. Additional concerns have been highlighted regarding the lack of cultural awareness and coordination with local authorities as well as international agencies 7,8,9. More recently, the response to the West African Ebola epidemic has shown critical gaps in the timeliness, coordination and effectiveness of international emergency medical teams responding to outbreaks 10.
The ‘Foreign Medical Teams’ (FMTs) initiative evolved in 2010 under the umbrella of the World Health Organisation (WHO), the Global Health Cluster and other actors, with the aim to improve the quality and accountability of international emergency medical teams responding to disasters. In 2013, the FMT Working Group published a first edition of the ‘Classification and minimum standards for Foreign Medical Teams in sudden onset disasters’, in which capacities, services and minimum deployment standards for FMTs were defined 11. A global list of quality assured and classified FMT organizations was launched in July 2015. A change of name from FMT to Emergency Medical Teams (EMT) with a pre-fix to differentiate International and National teams (I-EMT and N-EMT) was endorsed at the global meeting held in Panama in December 2015. This was in recognition of the importance of national and international teams working collaboratively to maximise the response to large scale health emergencies (Table 1).
Table 1. EMT and disaster related definitions
The World Health Assembly 2015 recognised the need for a global health surge capacity and the establishment of the Global Health Emergency Workforce (GHEW), of which the EMT initiative is a part. The GHEW aims to improve coordination, readiness and quality assurance in the deployment of EMTs and individual experts such as those deployed through the Global Outbreak Alert and response Network (GOARN) and other networks and partnerships 12.
To improve the quality and professionalism of deployed teams, a coherent approach to education and training has been identified as a key next step 8. A standardised learning framework is needed to assist EMTs to prepare for response and allow quality assurance mechanisms for the EMT initiative. Organisations wishing to be EMT classified will be required to reveal their training strategies.
Multiple organisations and universities have developed education and training programmes for disaster and emergency response; with a significant variation in scope, curriculum and quality 13,14,15,16. The lack of common standards to guide education and training design and provision have been highlighted 13,17,18. In addition, many of the proposed training models are focused on individuals, rather than multidisciplinary EMTs 19. The so called ‘competency-based models’ have been recommended as the basis for education and training in the disaster field by several authors 20,21,22,23,24,25,26,27,28. Such models are promoted as a way to standardise the training of individuals and contribute to the professionalisation of the discipline, but reviews of available competency models have shown limitations in their practical application 18,29. Although some authors have suggested possible ways to facilitate their alignment to practice 30,31, no competency models have led to a systematic and operationally focused framework to guide EMT organisations through an agreed training pathway for their teams.
The aim of this study is to explore and reflect on current practices related to disaster education and training and suggest key components for an operational EMT learning framework. This targets primarily I- EMTs.
Methods
This work has evolved out of the EMT process in which the authors are involved at different levels. The authors hold extensive experience in both medical field work in disaster contexts and disaster training development and implementation. Based on this, a first group (NAC, AH, IN, JvS) was formed to develop an EMT operational training framework that would contribute to quality and accountability mechanisms within the EMT initiative. A literature review was done compiling available literature from trainings and educational frameworks within the field of disaster medicine. Published literature search was performed using PubMed, EMBASE and Google Scholar. Since a limited amount of references about operational training was found, a search for grey literature followed. That included information from internet sites and other information made available for the authors by EMT organizations. The results were categorized and discussed by NAC, AH, IN and JvS, and a first draft with training recommendations was presented to the expert panel consisting of the remaining authors. Following sets of 5 revisions a final Global Operational Learning Framework was defined. The results presented are based on the discussion process that lead up to the framework.
Results
Current education and training for disaster and emergency response
Mainly individual education and training options are available to help prepare professionals engaging in disaster response. Individuals can strengthen existing professional skills and develop technical and context specific capacities through Masters level studies or short courses delivered by universities, training agencies or EMT organisations themselves, many of those trainings being recently compiled by Jacquet et al. 13. Two papers also gather a comprehensive compilation of postgraduate education programmes related to disasters offered in North America and Europe 14,15. Delivered online or face-to face, the numerous available courses cover multiple subjects; as broad as Global Health or as specific as nutrition or logistics in low-resource settings. The previously mentioned competency based models, mostly compiled in two systematic reviews 18,29, aimed to guide standardized curriculum design but their application in practical courses have not yet been documented. Training modalities also vary, from theory-based lectures and discussions, to case-scenario exercises and simulations 14,15.
Although it is acknowledged that EMT deploying organizations provide team training little evidence of their practices is available. The training approach followed by strong and experienced EMTs and organisations involved in emergency response have hardly been studied, even if many lessons may be learnt from their experiences. These organizations comprise emergency teams from international organizations, governments or well-known NGOs, as well as police, Fire and Rescue, ambulance services or militaries. They often follow an operational approach to training, immersing their teams into contexts they will likely be exposed to once in the field. Simulations, teamwork, pre-deployment preparation and the inclusion of regional and national actors are key features of their training practices 32,33. Table 2 illustrates some examples of these practices, which should be especially considered when designing an operational approach to training for EMTs.
Table 2. Examples of emergency training by relevant EMTs and emergency organizations
Recommendations for a global operational learning framework for EMTs
After a critical analysis and discussion around EMT education and training current practice and needs a systematic approach linked to current WHO EMT standards is presented. It recognises both individual competencies and team dynamics within the procedures of a field deployable agency as being equally important factors for an effective response.
1. Three-step learning process
The three steps proposed below (Figure 1) are designed to:

Fig. 1: Three-step learning process for EMTs
With different formats and levels of complexity, several authors have already mentioned comparable stages of competency, training and development 20,21,25,31. The classification suggested in this paper simplifies the current approaches and provides a clear picture of the minimum team capacities needed to deploy as an EMT, leaving space for the future design of pathways for those seeking sector professional development. As the three steps presented aim to be the minimum standard for education and training, no individuals should be deployed to the field without going through all steps; each being considered equally relevant for EMT performance during disasters. It is the responsibility of EMT organisations to ensure that staff has gone through all three steps. Well-trained EMTs will result in more effective performance and better care for populations affected, rather than just the career development of an individual.
Step 1 – Professional competence and license to practice
The core standards recommended within the 2013 publication ‘Classification and minimum standards for Foreign Medical Teams in sudden onset disasters’ 11 , already 7 underline the first step to consider in relation to EMT education and training: ‘FMTs must ensure all their staff are registered to practice in their home country and have licence for the work they are assigned to do during their deployment, as well as showing expertise in their field of practice’.
Although EMT organisations are not in charge of providing this education, they have the responsibility to ensure their staff have been trained and accredited by a competent authority for their field of health practice. This learning step must occur before a professional becomes part of the EMT. For example, an EMT member would comply with step 1 by getting a medical degree, a license to practice from their specific professional body and relevant working experience in his/her home country.
Step 2 – Adaptation to context
Another established core standard for EMTs 11 is the need to ensure members are appropriately trained for the context in which they will work. Step 2 of the recommended learning approach emphasises that EMT members must adapt exiting professional skills and competencies to the resource limited emergency contexts.
Step 2 training should be done well ahead of deployment. Courses and education platforms should besides professional context adaptation focus on developing skills to critically assess and analyse the situation in order to ensure that priority is given to the most essential health needs of the population and a capacity to triage, based on public health priorities and available resources. Examples of technical training courses are those providing context specific clinical skills (surgery, wound care, paediatrics, mass casualty), public health (disease prevention, health systems, management of epidemics) or logistics (shelter, water and sanitation). Examples of non-technical subjects include ethics, cultural awareness, leadership, communication or understanding of the humanitarian structure.
EMT organisations may have the capacity to facilitate this learning step internally, but can also use external partners, such as universities or training companies, to organise and deliver it to their EMT members. To receive step 2 education and training, 8 individuals could also enrol in existing university based Masters programmes or short courses related to disaster and emergency management or health in disasters.
Step 3 – Team performance
Previous professional expertise and the completion of emergency and low-resource adapted individual courses provide the basis for good practice in the field, but do not ensure the successful performance of a team deployed into a disaster 19.
EMT members need to prepare for their deployment as part of a multidisciplinary team integrated within an EMT deploying organisation. This training goes beyond the individually focused training of step 1 and 2 above, and puts teamwork and EMTs’ specific procedures into focus. All EMTs should offer pre-deployment courses in order to transfer to its members the values and mandate of the organisation, its main protocols, communication pathways, security guidelines, teamwork dynamics, basic aspects of personal health and travel, and other subjects related to deployment working and living conditions. This training must be practical and multidisciplinary, and inclusive of all health care workers and non-medical professions. It is anticipated that the team members who train together may not always be the same that deploy together; but a standardised pre-deployment course should allow those taken from an organisation’s roster to work as an effective team. Step 3 training is the responsibility of the EMT agency but may be delivered in partnership with other training providers.
2. Considerations for training delivery
From theory to practice
We assume both theoretical and practical learning to be a base for any professional field. In the initial phase, theoretical education facilitates knowledge acquisition, but soon trainees require more practical and hands-on training sessions in which to apply these theories. Following the same pattern, EMT learning process moves from theory to practice as deployment comes closer. Face-to-face or e-learning theoretical courses should then be followed by real or simulation based, practical training. Although it will be best to expose trainees to the real context of the disaster and emergency in which 9 they will ultimately be working, this is rarely possible. As an alternative, simulation based training can offer a feasible and effective approximation to real-life practice in the field 34,35,36.
The traditional real-life drills and table top exercises can be difficult to organise due to the length of time and amount of resources required for design, execution and review. Technologically based approaches to disaster training appear promising in their ability to bridge the gaps between other common training formats. For example, during the recent Ebola outbreak emergency, virtual reality (VR) training was designed by replicating an Ebola Treatment Centre (ETC) to create a safe and realistic environment in which trainees could gain realistic skills. Although it had some limitations, a VR training programme produced a cost-effective option and increased access to simulation training 37.
Although more costly, exposure of trainees to low-resource settings could be achieved through the establishment of field training facilities, similar to the Red Cross/ Red Crescent Field School included in table 2. Agreements between academic institutions and non-governmental organisations (NGOs) can offer similar opportunities. An example of this was a project in which online training was combined with a medical apprenticeship in low-income countries during an anaesthesia and intensive care medicine residency in Italy 38.
From individual to team training
Although the pursuit of individual expertise is important, the scale of disaster operations requires an organised response by teams of interdependent members, who can incorporate individual efforts into coordinated actions 39. Thus, understanding the roles of other professional groups included in the team and learning how to work together to reach a common goal are key aspects of a successful disaster response 40. Moreover, team training across different clinical contexts has proven to impact positively upon healthcare teamwork processes and it has been associated with improvements in patient outcomes 41,42. The team approach is also valid for the whole system responding to the disaster – i.e. working as a multidisciplinary and interdisciplinary team with national staff and other organisations.
While EMT training is mandatory it cannot replace experiential learning and field mentorship. The team composition should be considered carefully, with a balance between senior and junior staff that allows a quality performance of the team and the mentorship of its junior members. This is likely to be inappropriate in the first response team, but to be encouraged in second and subsequent staff rotations as a situation stabilises. This important recommendation is also recognised in the minimum standards for FMTs 11.
Just-in-time training
Just-in-time training (JITT) is recognised in medical education as a valuable and effective training method to disseminate newer concepts or seldom-performed procedures 43,44. Already suggested as relevant to EMT training 30, potential JITT modules will introduce additional skills and knowledge to the staff just before deploying into specific contexts – e.g. clinical management of Ebola patients or description of trauma national protocols of a disaster-affected country. JITT courses – short and well defined in their scope – could also be organised to present updates of former EMT guidelines and procedures, or refresh important concepts after a period without deploying to the field or since original pre/deployment training.
Skills mix and team composition
Training matrices can be used to identify which team members require which skills and to what depth of knowledge. The idea of team rather than individual skills development is important. A surgical team in a Type 2 facility for example must be able to perform emergency general surgical procedures such as a laparotomy for trauma, as well as wound and limb injury care that has orthopaedic and plastic surgical elements, and be able to manage an emergency caesarean section. In that case the organisation must decide to either bring a surgical team encompassing the different specialised surgeons or to bring generalist surgeons who have specific skills in each of these areas. Similarly all team members must be aware of safety and security procedures, but at least one person from the team should have in-depth knowledge of this area to support team safety and security planning and operations.
Need to complete all levels of training
Individuals or groups who were not self-sufficient in the field contributed to the chaos in recent disasters and added an inappropriate burden to the affected country without contributing to the care of the affected population. Academic institutions providing Step 2 education and training must guide their graduates on the appropriate mechanisms to deploy. If not there is a risk of encouraging more spontaneous and unsupported responders, in opposition to a systematic approach to emergency response led by wellprepared teams.
Recent EMT field deployments have exposed a lack of public health skills amongst some deployed clinical specialists, for instance during the Ebola outbreak, when public health understanding was especially relevant 45. This again reflects the need for a multidimensional learning framework in which contextual adaptation is crucial.
Next steps
The framework proposed in this paper – backed-up by international experts in the subject – encompasses existing successful initiatives where these principles have already been applied and documented in relation to EMT training, and complies with recognised WHO EMT standards. Although we believe this is a strong base for a global framework, its endorsement and testing by other EMT organizations should follow this publication.
This paper suggests the key components for an operational learning framework for EMTs but recommended curriculum content for each of its steps needs to be further defined and agreed. This should come with strong input from EMT organisations, rather than be driven solely by academic institutions. This could occur as a dedicated working group under the auspices of the WHO EMT initiative. The EMT WHO website could be used to share current education and training programmes by well-known organisations that could serve as guidance for other EMTs. Further development of open access training materials available to national and international EMTs will contribute to the quality improvement of the training practices.
Evaluation and accreditation of courses and participants remains an important area for discussion. The completion of exercises by trainees during a classroom course or a simulation exercise does not ensure they are competent to perform appropriately once in the field. Effective mechanisms to assess trainees´ capacities should be established. For example, training-participants’ performance during simulation exercises can be assessed through debriefing sessions, led by specialised facilitators who can challenge inadequate 12 practices identified and recommend improvements. Supervision and assessments during and after deployments can also contribute to the evaluation of the level of competence of EMT professionals once they are working within an organisation. Tools to allow meaningful and constructive debriefing and feedback from disaster affected countries also need to be developed. The establishment of a minimum dataset and uniform reporting, including collaborative and coordinated post-deployment research and evaluation, will strengthen the development of the learning framework.
Conclusions
Multiple attempts to standardise the education and training of disaster and emergency responders have been made; these focused mainly on an individual’s professional development rather than improved team operational performance. No agreed overarching framework currently guides EMTs through the principles of training or recommends suitable training methodologies. Since a systematic approach is needed, this report suggests a three-step operational learning framework for EMTs that could be implemented by EMT organizations globally. In addition, the importance of the training modalities used is highlighted; including individual and theory based education but emphasising team and practical simulations as crucial to the operational nature of an EMT’s work. Further work is required to fully develop an agreed curriculum and open access training materials for EMTs. These training materials will also contribute to the development of N-EMTs, some of which may be offered to neighbouring countries as IEMTs. WHO, EMT organisations, universities, professional bodies and training agencies can all contribute to the development of professional and highly functioning teams, but should recognise that only a collective approach will improve EMT field performance and crucially, result in better care for the victims of large scale health emergencies.
Competing Interests
The authors have declared that no competing interests exist.
Data Availability Statement
All relevant data are within the paper.
Corresponding Author
Ian Norton
Contact e-mail: [email protected]
The 2016 World Humanitarian Summit Report Card
The World Humanitarian Summit (WHS) in Istanbul took place on May 23-24, 2016 with 9000 attendees from humanitarian aid and disaster relief organizations, crisis-affected countries and governments. It was in part prompted by the terrific flow of refugees from the Middle East to Europe, the growing gap in being able to meet the needs of displaced peoples affected by conflict and disasters and the realization that broad reform is essential to move forward.
The UN Office for the Coordination of Humanitarian Affairs (OCHA) conducted pre-WHS consultations with non-governmental organizations (NGOs), academia, youth, and the private sector on 13 October 2015. This was followed by a global meeting on 14-16 Oct to capture the opinions, ideas and voices of the multitude of stakeholders. 1,2
OCHA attempted to attract a large number of global leaders to the summit with all indication of conducting a formal intergovernmental process. However, when only 50 non-G7 leaders indicated attendance,3 representing a paltry 5.2% of the global population, it may have determined that an ‘unofficial’ exploratory approach would be more useful in advancing the reform agenda at this stage in the process. Unfortunately, nation states prefer to participate when the outcomes are clear and may have felt disinclined to attend due to a lack of extensive political involvement and dialogue.4 However, the tightly orchestrated program left little room for exploration and emerging issues had to be discussed in casual conversation.
Based on the outcomes of the pre-WHS process and the resulting agenda and participant list, some decided not to attend. Most notable was the absence of Médecins Sans Frontières (MSF), which was frustrated by the lack of attention to international humanitarian law and civilian protection – two issues that greatly affect its own ability to operate and function effectively in conflict-prone environments.5 In 2015, 150 health facilities had been bombed, and in Syria over 220 systematically targeted attacks were launched on separate medical facilities making a shambles of any “law of war” protections in the 21st Century.6 The inclusion of these elements was a reasonable expectation since the summit was oriented towards organizations engaged in humanitarian assistance, which needs to be bundled with legal and physical protection. Likewise, this neglect was a slight on cooperation with the security sector, which is invariably called upon for assistance as soon as governments and NGOs cannot cope. Clearly, today’s wars are pursued on the same barbaric belief last seen centuries ago: ‘the more egregiously and violent the war is waged the shorter it will be.’
Conflict results in displaced peoples crossing borders and subsequent international assistance. Much of what happens in humanitarian action is thus about politics and security, which requires the support of international law and the enforcement of accepted standards. Nevertheless, no clarity was forthcoming on the required conditions that must exist for a UN agency to initiate humanitarian action and exactly what relevance the Geneva Convention requirements have today. Without these issues of law being resolved, the protection of assisters and the assisted continues to be problematic.
The organizers made the best of the situation and abandoned the prospect of political solutions and serious reform in favor of smaller, more achievable objectives. The outcomes reflected this predicament and manifested in the form of many fairly technical commitments, such as the ‘Grand Bargain,’ the name given for a package of reforms to humanitarian funding designed to make humanitarian assistance more ‘effective and efficient.’ However, despite considerable attention to technical financial solutions, the reforms were accused of being watered down during the negotiation process. Not much emerged to fill the humanitarian aid gap or address the need for flexible multiyear financing and longer time-frames. It is hoped that efforts will now turn towards monitoring action and accountability to avoid depressing effects on the ground.
There were also very positive outcomes with promising endeavors in the areas of localization, innovation and education. A fundamental shift on how to provide humanitarian assistance, especially in situations of protracted conflict, was promoted in a new business model for the sector. The UN and international donors were asked to move from ‘What action we take’ to ‘What action you take with our support’ to foster action by local organizations. The WHS provided a platform for an international conversation by humanitarian practitioners on the need for change and its endorsement of this shift lends the process new energy and direction. Under the Emergency Medical Team movement, local and national capacity should grow in leaps and bounds once the UN and other local, national and international humanitarian players adopt this model.7
This shift in the way that humanitarian assistance is provided is nothing new and some organizations have been transferring the burden of local effort to local organizations for a long time while they move command and control further afield. Other trends in innovation, recognizing the role of education and the relief-development relationship in protracted conflict and urban situations were inspiring.8
It is argued that the formal humanitarian system “faces a crisis of legitimacy, capacity and means, blocked by significant and enduring flaws that prevent it from being effective”.9 This is not only due to increased frequency, magnitude, severity, duration and complexity of crises. It is due to the UN failing to follow its own principles and breaking its own system.
Unfortunately, following the WHS, a scathing report revealed that the UN, by abdicating control of the delivery of aid in Syria to the Assad government, is in serious breach of the humanitarian principles of impartiality, independence and neutrality directly resulting in the prevention of aid to those most in need.10 In the 1980s in Africa, subsequent Security Council resolutions sanctioned government interference in the delivery of food and medical aid. This resulted in unmitigated civilian deaths and starvation, but the UN has repeated this breach of principle. This represents a dramatic departure from the first goal of the WHS to “Reaffirm our commitment to humanity and humanitarian principles”11 and the second core responsibility – to “uphold the norms that safeguard humanity.”2
The WHS was in a way, recognition that the humanitarian system is dysfunctional. It encouraged the participation of a large number of people to foster open and productive dialogue in a massive information-sharing endeavor. It facilitated explicit and elevated, sector-wide, formal and informal policy discussion on humanitarian systems, structures and funding.8 However, it failed to adequately address systemic issues and focused on piecemeal technical solutions.
Humanitarian aid is no longer only about the UN and donors. We need to move away from the current highly centralized model in which local and national NGOs only receive 0.2% of OECD Development Assistance Committee aid funding while UN agencies receive the bulk.9 A naturally evolving ecosystem of diverse actors that collectively represent and work for common humanitarian objectives is arising. The need to identify how to work cooperatively is driving the call for reform, which is the next logical step that will influence how civil society, political entities and the security sector work together in the years to come.
The WHS was successful in promoting the idea of local ownership and leadership in humanitarian action, and this is an essential precursor to a structural reform of the humanitarian system. The summit has created pressure for change that is expected from the next, soon to be elected UN Secretary General. Subsequent reform meetings should focus on why the current humanitarian system exists, who it serves, what behaviors it encourages, how this impacts on the delivery of aid, how the world has changed, and how humanitarian standards and laws need to evolve to continue to be relevant and functional. While powerful political support is required, it is the donors that hold the purse strings and it is them that need to support this reform.
We need a global humanitarian body employing a decentralized operational model to manage the flow of funds from governments and the cloud, and coordinate international responses. Such an agency would be able to end the divide between aid organizations and the security sector and would cater not only for people affected by conflict, but also disasters. Such an agency would be able to step in when small nations are unable to coordinate responses to overwhelming crises. The over 210,000 people working in humanitarian assistance also need legitimization which can be achieved by professionalizing the humanitarian occupation.12,13 The UN has demonstrated a failure to commit to its own humanitarian principles and is no longer qualified to lead this effort without far more significant reform.
]]>Method: This article briefly reviews current practices of analytical tools such as probabilistic cost-benefit analysis and identifies issues associated with its applications in small scale community based DRR interventions.
Results: The article illustrate that while best scientific knowledge should inform policy and practice in principle, it should not create an unrealistic expectation that the state-of-the art methods must be used in all cases, especially for small scale DRR interventions in developing countries, where data and resource limitations and uncertainty are high, and complex interaction and feedback may exist between DRR investment, community response and longer-term development outcome.
Discussion: Alternative and more participatory approaches for DRR appraisals are suggested which includes participatory serious games that are increasingly being used to raise awareness and identify pragmatic strategies for change that are needed to bring about successful uptake of DRR investment and implementation of DRR mainstreaming.
]]>Introduction
Amid the rising costs of natural disasters observed globally, emerging international consensus holds that a primary remedy to the lack of appropriate risk management – and ex-ante disaster risk reduction (DRR) investment in particular – can be found in better communication regarding the cost-effectiveness of DRR investment 1,2. Over the past two decades, natural disasters have affected a total of 4.4 billion people worldwide, causing as much as $2 trillion in economic losses 3. By 2030, accelerating urbanization, continued asset build-up in hazard-prone areas and other adverse consequences of poorly managed development are expected to double the economic losses from natural disasters globally4. To curtail these trends in risk creation, ex-ante quantification, evaluation and the integration of disaster risk into development are increasingly seen as crucial. ‘DRR investment saves’ has been a major slogan in such discourse, where the lack of awareness and scientific evidence are seen as the major obstacles hindering the rational decision to invest in ex-ante protection of our wellbeing, livelihoods and productive assets5.
The general premise that improved risk knowledge will lead naturally to enhanced DRR investment is not only theoretically debatable6 as has been critiqued by numerous behavioural and political economic studies which explain why we continue to underinvest in DRR despite the knowledge of its net benefits7,8 ; it has also created a practical issue in which increasingly sophisticated enquiries – often beyond the capacities of developing country practitioners – are called for to present scientific evidence regarding the costs and benefits of DRR investment 9 . While the concept and use of evidence-based assessments is advocated, the practical challenges of implementing such analyses in developing country contexts are, until today, insufficiently acknowledged.
A quantitative method known as probabilistic cost-benefit analysis (CBA) is often considered the state-of-the-art in the appraisal of DRR policies, in which probability distributions relating hazard return periods and loss estimates are calculated 10. The use of such CBAs has expanded considerably in the recent years where not only large scale public investment, but also smaller community-scale DRR interventions are increasingly evaluated using this methodology 11,12,13. Despite the considerable complexity, uncertainty, resource requirements, common measurements such as benefit-cost (B/C) ratio and Net Present Value (NPV) have routinely been used to justify, and raise awareness for, an increased investment in ex-ante DRR13 .
Calls for more sophisticated risk assessments, especially in light of climate change, however begs a number of pragmatic questions – such as whether or not sophisticated quantitative appraisal tools are effective in raising policy awareness and what alternatives are available. These questions are particularly germane in the context of developing countries where data and resource limitations, computational needs and uncertainty are high, and complex interaction and feedback may exist between DRR investment, community response and longer-term development outcome.
When risk-based decision tools should be more than awareness-raising
‘DRR investment saves’ is hardly a new story: good technical evidence exists within developed countries 14, and more stock-taking are recurrently taking place in developing countries 12,13 . Moreover, what researchers have learned over the years is that the core issues behind continued under-investment in DRR are more than the lack of knowledge: not only cognitive issues, but behavioural gaps of failing to act, institutional barriers of not having appropriate mandates, and other political economic barriers all hinder DRR uptake. Therefore, using alternative and more sophisticated appraisal approaches per se is unlikely to help. While CBA has been frequently required by national and international bodies, available evidence suggests this has led to limited learning during project appraisal and implementation15 .
The true utility of appraisal methods such as CBA will likely be realized when it is used for tangible policy and investment decisions rather than mere awareness-raising. However, there are a number of practical challenges for such tangible application in developing countries. The lack of local capacities to collect and analyse hazard-, exposure- and vulnerability information is a major issue: whether downscaling efforts are made to climate hazard estimations or national average parameters are used to construct particular cost estimates, these will all contribute to increasing uncertainty bounds, and making proper sense of such uncertainty becomes a big challenge. Moreover, as these efforts require highly sophisticated analytical skills, which are often handled by external consultants, thereby removing the process of evaluation from community deliberation and learning. Methods such as CBA can be conducted in a participatory manner 16 , however, this often involves an elaborative process and learning potential may be limited. CBA is of course hardly immune from the usual caveats in the developing countries, including the lack of consideration for distributional consequences, limited applicability of shadow pricing, issues of high discount rates and costing of intangibles 13 .
At what cost?
Given the complexity and uncertainty involved, it is unlikely that such a sophisticated approach will be appropriate for all cases, especially for small scale DRR project appraisal in developing countries. Missing reliable past disaster damage and loss estimates, probabilistic assessment of community-based interventions often rely on local knowledge: the establishment of baseline risk from annual to 2-5 year events may be feasible based on local residents’ recollection, however such methods quickly become infeasible for higher return period events such as 100 or 500 year events that are needed to accurately estimate the risk of extremes.
Furthermore, these issues are compounded when the appraisal is required to integrate the future impact of climate risk, which is particularly uncertain at the local scale. This requirement may be understandable when donor funding is extended under climate change adaptation. However, when such demands are made on tools such as probabilistic CBA, it adds a further layer of uncertainty on top of the existing hazard variability and local exposure and vulnerability dynamics which themselves are often poorly understood. Even in ideal circumstances, state-of-the art risk assessments are limited int their ability to offer robust future forecast, since the further they need to project into the future, the larger the uncertainty bounds become for hazards, exposure and vulnerability. Finding meaningful interpretations therefore becomes progressively difficult.
When not all evidence has to be numbered
In light of these practical constraints, communities may instead use more locally appropriate methodologies to raise awareness and to plan for improved DRR practice in the context of climate change. Practitioners may raise local awareness regarding the effectiveness of ‘soft’ DRR measures vs. ‘hard’ DRR measures, by simply comparing the direct damages avoided such as crop loss, human injury and the deaths avoided based on the knowledge of past disaster events.
Furthermore, interactive methods such as participatory ‘serious’ gaming may be used to address existing barriers and uncertainty. Instead of reducing DRR benefits and costs into a single metric such as B/C ratio and NPV, this type of participatory analysis takes the advantage of its complexity and uncertainty – by turning them into a fun and creative virtual space where community members and practitioners together explore potential solutions for DRR. These system-thinking based tools can be used to identify barriers to action such as cognitive and behavioral stumbling blocks (e.g. resistance to changes and deviation from existing practices and social norms) or institutional and political barriers that may challenge the implementation of DRR17,19,21,22,23 . These types of approaches are particularly effective at challenging the many preconceived notions that are at the heart of policy inaction: as a recent study of game-based study in Mozambique, Uganda and Ethiopia show those who saw nothing but obstacles to change prior to gaming-interventions were able to identify and implement pragmatic changes to their community adaptation planning such as involving wider sectors in discussions and designing DRM plans based on potential, as opposed to past, hazard occurrence.21 Prior understanding of institutional and social contexts are crucial in designing and implementation and communications and reflections during and after gaming-sessions are one of the most important element in bringing about attitude, behavioral and institutional changes.21,23 The training needs for skilled facilitators and time commitment of community consultations are of course high, but another strength is that these types of analyses may be built upon existing monitoring and evaluation techniques used by community-based practitioners such as vulnerability and capacity assessment (VCA)11,18 .
Awareness-raising and appraisal tools—getting our expectations right for Post-2015 DRR agendas
Looking beyond 2015, the demand for risk-based decision-making will likely increase. While best scientific knowledge should inform policy and practice in principle, it should not create an unrealistic expectation that the state-of-the art methods must be used in all cases. If decision-making tools, such as probabilistic CBAs, are to be useful (rather than be constraining), there are number of areas where further research and capacity building are required. First and foremost, the use of quantitative risk appraisal tools at community levels should be viewed as a vehicle for engagement and learning. We must critically reflect on why we continue to under-invest despite our existing knowledge that DRR saves in the longer run, and make adjustments to our strategies accordingly. Second, for such tools to be useful beyond awareness raising, further efforts are certainly needed to systematically develop capacities and to collect locally applicable data in developing countries. Emerging initiatives such as crowd-and-expert-sourced hazard, exposure and vulnerability for example, offers potential avenues to collect risk information in data scarce environment.24 Thirdly, it is important to understand that sophisticated quantitative focused tools are not appropriate in all DRR investment appraisals. Depending on scale and scope, less demanding and more qualitative and creative appraisals may be better able to deliver meaningful assessments. Of course, this does not mean we can forget about risk and probability all together – we need a nuanced approach when integrating expert and local knowledge and learning for effective co-production of DRR solutions. Further research and capacity building will certainly be helpful to develop and test alternative evaluation methodologies and building robust empirical evidence in developing countries.
Competing Interests
The authors have declared that no competing interests exist.
Background
Hazardous chemicals and radioactive materials – collectively called hazardous materials for the purpose of this paper – pose serious threats to public health by accidental release or intentional dissemination. Many such substances are present in large quantities throughout the world, as they are used in common industrial, energy-producing, household, and other processes. Terrorists have also manufactured and/or weaponized certain hazardous materials for the purpose of intentionally harming civilians. The risks are illustrated by past incidents, both accidental and intentional, such as the release of methyl isocyanate from a chemical plant in Bhopal, India in 19841, the attacks by the cult Aum Shinrikyo on Japanese civilians with the nerve agent sarin in 1994 and 19952, and the earthquake-induced damage and core meltdown of the Fukushima Daiichi nuclear power plant in Japan in 20113. Each of these incidents caused exposure of dozens to thousands of people to hazardous material.
In this type of scenario, people can become contaminated by the hazardous material(s) through various routes of exposure, potentially leading to severe adverse health effects. External contamination may result from airborne release of a hazardous material which is then deposited on skin, eyes, hair, and/or clothing; or it may result from a person’s direct contact with a liquid or solid substance which gets transferred to skin, eyes, hair, and/or clothing. In either case, if not removed, the contaminant can be absorbed into the body through the skin or eyes and cause toxicity. Contaminant on a person’s skin, hair, or clothing also presents risks of inadvertent ingestion or re-aerosolization followed by inhalation. Once a hazardous material is ingested, inhaled, or absorbed through the skin or eyes, it is considered to be internal contamination. Decontamination – any process, method, or action that leads to a reduction, removal, neutralization, or inactivation of contamination – prevents or limits absorption of external contamination into the contaminated person’s body and also prevents transfer of the contaminant to other people and objects. Decontaminating an individual who is externally contaminated with a hazardous material, therefore, protects the individual’s health as well as the health of other community members.
Heightened concern about the risk of terrorist attacks causing mass casualties with chemical, biological, radiological, or nuclear agents, as well as initiatives to prepare for large scale chemical and nuclear accidents, have driven investments in equipment and efforts to develop capabilities for decontaminating large numbers of people in a rapid and efficient manner. For example, within the United Kingdom (UK), England’s Department of Health and equivalent structures in the devolved administrations of Northern Ireland, Scotland, and Wales purchased mobile decontamination units and distributed them throughout the country4. The United States (US) Hospital Preparedness Program in the early 2000s required awardees to ensure that adequate portable or fixed decontamination system capability existed statewide.
However, mass casualty decontamination methods, practices, and equipment have evolved with sparse science to shape them. Insufficient attention has been devoted to defining mass casualty decontamination goals and subsequent analysis of how to integrate decontamination into an emergency response in order to best achieve those goals. A contaminated casualty, emergency responders, and bystanders are all potentially at risk of adverse health effects from the contamination. There is an urgency to decontaminate in order to reduce a casualty’s further exposure to a hazardous material, if the substance can enter the body readily. This may have to be weighed against the highest priority demand to provide other life-saving medical treatments and supportive care. At the same time, emergency responders and hospital personnel must protect themselves from becoming contaminated. Furthermore, the most appropriate response approach will depend on the nature of the incident. For example, exposure to a gas or vapor can be limited by actions other than water-based decontamination, including moving people away from and upwind of the point of release and removing clothing. A range of exposure levels may result from a hazardous materials release; in a mass exposure incident, responders and hospital personnel will need to make decisions in order to categorize and prioritize people for decontamination, including those who do not need decontamination at all. Little evidence is available to guide the risk assessment and decision making, or triage, that are vital for achieving the goals of casualty decontamination.
Evidence is also lacking to suggest the best ways to conduct decontamination once the decision to decontaminate has been made. For example, optimal conditions for applying water-based decontamination to diverse civilian populations (including children, pregnant women, elderly, and others) contaminated with various hazardous materials using different types of equipment have not been well delineated. Circumstances in which water-based decontamination should not be conducted, such as in cold weather, when the risk of hypothermia is high, and what alternative processes should be used need to be identified. Although health outcome-based goals have been defined for radioactive contamination, they have not been established for chemical contamination. It follows that metrics for determining the effectiveness of decontamination in a chemical incident are lacking. Assessing the evidence from experimental research and actual incidents could help to identify decontamination methodologies that may be effective in both chemical and radiological incidents as well as aspects of each type of incident that require a unique approach.
Toxic chemicals and radioactive materials differ in some physical or chemical properties that translate into distinct health risks when a person is externally contaminated. Many chemicals are readily absorbed through the skin, and, within certain limits, as the amount of chemical absorbed increases, the toxic effects increase. Chemical contamination, therefore, poses an acute health risk to the contaminated person him/herself. External chemical contamination of an individual creates additional public health risks by presenting opportunities for the spread of contamination to emergency responders, hospital personnel, and health care infrastructure. By contrast, most types of radioactive material do not readily cross through the skin, with a small number of exceptions such as tritium and, to a lesser degree, radioiodine. Certain beta emitters can also be exceptions; when deposited on the skin they may cause skin burns, which can lead to systemic contamination if the beta emitters enter the body through the burned skin. Wounds or otherwise impaired skin also may allow easier entry of radioactive or chemical material into the bloodstream than intact skin. Overall, however, external radioactive contamination presents much less of an acute health risk to the contaminated individual than chemical contamination. Rather, the primary health risk associated with external radioactive contamination is that it can be internalized through ingestion or inhalation. A contaminated individual can inadvertently ingest or inhale the contaminant directly and/or spread the material to other people and objects, causing secondary exposure.
Decontamination of the contaminated individual mitigates health risks to the contaminated individual and to others to whom the contamination could spread. Yet, casualty decontamination must be integrated with other aspects of the response. The nature of the contaminant helps to determine response priorities and their urgencies. Many chemicals are quickly absorbed and begin to exert their deleterious effects within very short times, on the order of minutes to tens of minutes. Casualties may need both decontamination and medical treatment, such as administration of a therapeutic pharmaceutical or supportive care, urgently. Decision making is usually necessary at the time of the incident to choose a response strategy that is most appropriate for the situation. For known radioactive contamination, recommended response strategies are better defined and priorities have been easier to establish in pre-incident planning than for a chemical incident. This is due to the relatively low likelihood of acute adverse health effects from external radioactive contamination as well as the widespread capability among responders to measure radioactive contamination and compare it to established acceptable levels. The hazard presented by radioactive contamination is not considered significant enough to warrant a delay in the administration of life-saving medical treatment, if needed, in order for the individual to be decontaminated5 (International Atomic Energy Agency, 2005). However, the specific identity or even the general nature of the contamination in a hazardous materials incident may not be known immediately. Emergency preparedness and response communities may benefit from comparing the evidence and harmonizing approaches, when appropriate, between chemical and radioactive contamination incidents, forging the way for an optimised, albeit generic, approach.
Advances have been made in the science and practice of mass casualty decontamination in recent years. Research teams in Europe have conducted well designed studies, the results of which have been incorporated into best practice guidelines for European countries6. A group in the UK is currently funded by the US Department of Health and Human Services to continue studies of the conditions for the most effective water and soapy water-based decontamination. Hazardous Area Response Teams (HART), who can provide life-saving medical care in a hot zone or other non-permissive environments, now operate in most major cities in the UK. Similar response services are being rolled out in other regions of the UK. The French plan for responding to an urban chemical attack also provides for specially trained physicians, paramedics and firefighters to administer life-saving medical treatments before and during decontamination7,8,9. The Japanese government published official decontamination guidelines in 2004, which are regularly tested in joint civil protection exercises involving local and national governments. Germany also developed an updated concept for the decontamination of casualties exposed to hazardous materials. In 2005, the International Atomic Energy Agency and the World Health Organization published an emergency preparedness and response guide for the medical response to a nuclear or radiological emergency5. The US has also provided recommendations on using firefighting equipment for mass decontamination10 and evidence-based national planning guidance for conducting mass casualty decontamination in a chemical incident11. There has been consideration of strategies for both self-care decontamination (Monteith and Pearce, 2015) and responder management of the public (Carter et al., 2015) during mass exposure chemical incidents. A PubMed search reveals that in 2015, papers were also published by researchers in several countries on specific technical aspects of decontamination, such as hair 14 and wounds 15,16, together with studies exploring the efficacy of novel decontamination products 17,18 and Reactive Skin Decontamination Lotion 19.
These are examples of recent progress; however, significant knowledge and planning gaps remain. Research is needed to identify strategies for conducting decontamination of a heterogeneous civilian population that is likely to consist of the young, pregnant women, the elderly and frail, as well as a mixture of individuals of differing ethnic and cultural backgrounds, collectively contributing to susceptibility. Decontamination, therefore in a mass exposure incident, must take account of these factors to yield the best health-based outcomes. Evidence-based guidelines should be published and incorporated into plans and training curricula by local response organizations. A more intensive, concerted, and sustained effort supported by health policy and emergency preparedness decision makers is needed to address these gaps and enhance preparedness for mass casualty decontamination.
The Global Health Security Initiative (GHSI) is an informal network of countries formed in 2001 to ensure health-sector exchange and coordination of practices in confronting risks to global health posed by chemical, biological and radio-nuclear threats, as well as by pandemic influenza. The member countries/organizations of the GHSI are Canada, France, Germany, Italy, Japan, Mexico, the United Kingdom, the United States and the European Commission. The World Health Organization (WHO) is a technical advisor. As part of the GHSI partnership, an annual meeting of Health Ministers is held to foster dialogue on topical policy issues and promote collaboration. Other initiatives involving senior health officials as well as policy, technical and scientific personnel take place on a regular basis, focused on risk management; communications; chemical events; radio-nuclear threats; pandemic influenza; and global laboratory cooperation. The GHSI Chemical Events and Radiological/Nuclear Threats Working Groups, based on a series of workshops that included additional subject matter experts, have developed recommendations on the fundamental principles that should guide mass casualty decontamination in a chemical or radiological/nuclear incident and on areas of research that could drive improvements in mass decontamination effectiveness and efficiency. The scope of the work presented here is chemical and radioactive materials. Biological agents also pose important risks which may necessitate patient decontamination. In future work, these guiding principles and research needs can be built upon to address biological agents.
Guiding Principles for Conducting Mass Casualty Decontamination in a Chemical or Radiological/Nuclear Incident
GHSI subject matter experts wish to highlight the following fundamental concepts. The principles should be applied flexibly, using expert judgment shaped by the circumstances, and according to a country or local jurisdiction’s laws, regulations, policies, and resources. For additional information, please refer to the following documents, as well as other country-specific or international guidances:
Generic procedures for medical response during a nuclear or radiological emergency (International Atomic Energy Agency, 2005)5
Patient Decontamination in a Mass Chemical Exposure Incident: National Planning Guidance for Communities (United States Departments of Homeland Security and Health and Human Services, 2014)11
Initial clinical management of patients exposed to chemical weapons (World Health Organization, 2014)20
[1] Medical countermeasures include both pharmaceutical interventions, such as vaccines, antimicrobials, antidotes, and antitoxins, and non-pharmaceutical interventions, such as ventilators, diagnostics, personal protective equipment (PPE), and patient decontamination that may be used to prevent, mitigate, or treat the adverse health effects of an intentional, accidental or naturally occurring public health emergency22. In some settings, casualty decontamination is characterized as a protective action, which is encompassed by the broad definition of medical countermeasure cited here, as it can prevent adverse health effects in the exposed individual as well as in other people to whom the contamination could spread.
Priority Research Needs
Decontamination of casualties in a mass exposure incident has only recently begun to gain wide acceptance as a medical and public health countermeasure; thus, many questions about its optimal utilization have not been explored. New research and analysis would allow more evidence-based mass casualty decontamination practices to be established 11,23,24,25,26. Three broad topics have been identified by GHSI subject matter experts as priority targets for rigorous scientific investigation.
Operational analysis to determine the best ways to integrate casualty decontamination into the incident response and coordinate it with medical evaluation and treatment. Various ways of organizing a response to incorporate mass casualty decontamination have not been compared for their efficacy in mitigating morbidity and mortality. Evaluation of exercises and training, as well as other types of operational analysis and research could lead to better understanding of the most effective ways to achieve such integration. Decision support tools are needed to help guide decisions during triage on if, when, and how to decontaminate casualties, and how decontamination will be coordinated with medical evaluation and treatment. The logistical challenges of having medical countermeasures available and responders administering them in the field while wearing appropriate personal protective equipment should be included. This work should also take into account country, region, state, and other locality specific laws, regulations, organizational structures, practices, and other considerations that could limit the generalizability of mass casualty decontamination strategies.
Comparative study of the efficacy of various decontamination methods and their potential adverse effects. Limited research has been conducted on technical casualty decontamination methods, such as the optimal parameters for water-based decontamination. A US-funded project currently underway by UK researchers is assessing the effects of certain variables, such as water flow rate, temperature, and detergent type, on decontamination efficacy and adverse effects using a firefighting equipment-based decontamination system. This work will need to be extended and expanded with future studies, since many factors contribute to the way that water-based decontamination is delivered. An extensive body of work may be required to identify optimal parameters for maximizing efficacy and minimizing adverse effects. Water and soap have been demonstrated to effectively decontaminate skin contaminated with radionuclides.
Behavioral, communication and privacy issues: what do casualties and community members need and how to meet those needs in ways that will best support compliance with and effectiveness of casualty decontamination. Various communication, behavioral and social factors can significantly influence people’s actions during a disaster, yet strategies for using these factors to optimize compliance with and effectiveness of decontamination have not been thoroughly studied. UK researchers have begun to investigate the effects of various types of instructions provided to casualties undergoing decontamination 27, while Canada has considered how to provide psychosocial support to people who need decontamination during a radiological, nuclear, or chemical emergency 28. However, as with technical decontamination methods, communication is shaped by multiple factors and plays a role throughout the decontamination process. Enhanced decontamination effectiveness depends on coupled study of behavioral, communication, and privacy issues with technical methods and requires additional attention.
Conclusion
The GHSI Chemical Events and Radiological/Nuclear Threat Working Groups have identified current challenges to effective casualty decontamination in a mass exposure incident. Application of the guiding principles described here to preparedness, planning, and response activities will help to improve effectiveness of decontamination as well as other aspects of the medical management of casualties in a mass exposure incident, based on our current scientific understanding. Research programs designed to address the priority research needs will strengthen the scientific evidence, upon which further improvements in preparedness, planning and response can be based.
Competing Interests
The authors have declared that no competing interests exist.
Perspective
In recent years, evidence has emerged that disaster management places significant burdens on those tasked with carrying out planning, response and recovery functions, especially where human contact is involved1,2,3. Research has identified that rescue and recovery workers engaged in disaster relief are at increased risk of developing mental health problems such as post-traumatic stress disorder, depression and anxiety4. They are also at increased risk of empathy exhaustion, burnout, compassion fatigue, and vicarious traumatisation5. In addition to this, an increasing number of hereto thought of low-frequency-high-impact events has placed further pressure on resource allocation issues, as well as calls and new frameworks proposed for reform about how disasters are managed in the context of sustainable economies in the face of climate change at local, regional, and global levels (e.g. Sendai Framework for Disaster Risk Reduction 2015-20306).
The challenge of approaching disaster management across all sectors of society and the economy while paying attention to the human impacts of identified risks and as well as the impacts of preferred mitigation solutions is a mammoth task of scale and coordination. Implementing a framework to meet these challenges is an even bigger task.
In the health sector, patients problems are becoming increasingly complex and the care provided for them more and more fragmented. Efficiency savings, greater population disease burden, and constant pressure for cost savings place increasing pressure on resources, along with strain on relationships between staff members, and staff and the patients they care for. We know that all staff members in the healthcare professions are affected by the emotional demands of caring for patients. Whether this shows itself in increased rates of work related anxiety and depression absentees, or staff burnout, both clinical and non-clinical staff are at risk. In such circumstances, it has been noticed that care can become rapidly depersonalised with sometimes catastrophic consequences7.
One possible solution to this sense of depersonalisation and burnout has emerged from the experiences and writing of Ken Schwartz. During a harrowing 10-month ordeal before Schwartz died of advanced lung cancer, he recorded his reflection that what mattered most during an illness is the human connection between patients and their caregivers. In his book, ‘A Patient’s Story, he encouraged healthcare professionals to stay person-centred: “…the smallest acts of kindness”, he argues, make “the unbearable bearable”8.
Schwartz recognised that one way of supporting staff through the brutality of their everyday experience was to give them the space to reflect and talk – a space to be able to tell stories about things that happened to them during their work. The mission of the Schwartz Centre for Compassionate Healthcare, established after Ken Schwartz’s death, was to promote compassionate care so that patients and their caregivers relate to one another that offers “hope to the patient, support to caregivers, and sustenance to the healing process”8.
Schwartz Centre ‘Rounds’ are a multidisciplinary forum designed for staff together once a month to discuss and reflect on the non-clinical aspect of caring for patients, that is the emotional and social challenges associated with their jobs. Schwartz Rounds have been successfully running in hospitals in the USA for over 17 years, and have also been used to good effect in the UK9. The general format of Rounds is as follows: a pre-selected panel spend 10-15 minutes presenting a case story and describing their role, the issues the case raised for them, and how this made them feel. It is critical not to be diverted into the technical aspects of the case, as per a usual hospital Case Round, but to remain with the how the case made them feel. Under the guidance of a skilled facilitator, discussion then opens up to the larger group of participants for the remainder of the hour long meeting, asking questions to encourage sharing of experiences and to reflect on the challenges of care. Rounds are designed to be a safe, confidential environment that are not designed to focus on problem solving, but to instead to consider the implications of the case for staff. Rounds are generally held over lunch, with food provided for staff (which seems to be a critical part of the Rounds’ recipe for success).
The underlying premise for Rounds is that compassion shown by staff can make all the difference to a patient’s experience of care. In order to provide care with compassion, however, staff must in turn feel supported in their work. What the Schwartz Centre promotes is no ordinary ‘debriefing’ experience. In broad terms, staff are unprepared for and unaccustomed to reflective practice. Staff are rarely encouraged to stop to consider how their work feels, or what it means to do the work they do, for example, the ethical dilemmas, the existential issues of dealing with life and death, or the day-to-day stresses and rewards.
Schwartz Rounds are not intended to produce actionable outputs at the end of the process. Instead, their value lies in the process of both recounting the story from an overtly subjective point of view, and the act of listening and responding. These spaces are intended as times to be able to recognise and discuss the processes that healthcare workers find themselves deeply involved in. They provide an opportunity to share narratives with one another, and provide an experience through which to socialise us to be able to do so.
Staff who have participated in rounds report that they feel better supported in their patient care, and their levels of stress and isolation have been shown to decline. Furthermore, it was found that the more rounds attended, the greater the positive impact on staff10 and it seems that the very act of attending Rounds regularly focuses staff attention on the need for compassion. A separate study of regular Rounds attendees concluded that compassionate caring requires “a lifetime of continuous support”11.
In the field of disaster management, Schwartz Rounds have been used with some success. In July 2014, the Schwartz Centre published a White Paper describing how the protocol was used to help caregivers to collectively process the complex and challenging feelings and emotions that may arise when caring for the injured and dying after a traumatic event – in this case, the Boston Marathon bombing12. It is notable that one of the facilitators observed how she was struck by the fear that people were facing about attending the race one year later, indicating that they were not just processing the past but also facing the fear that something dangerous could also happen in the future12.
The World Conference on Disaster Risk Reduction in Sendai6 recently issued a 15-year action plan urging countries forward on several fronts. Five of the seven targets identified are particularly relevant for health. Moreover, this Framework is only one of four global level deals to be finalised this year, the others being on sustainable development and climate change, as well as the first World Humanitarian Summit in 2016. More and more targets and processes continue to emerge that place ever increasing burdens on disaster management staff, in all parts of the policy and practice arena
There is a risk that in focusing on the delivery of actions related to these international frameworks that disaster management becomes depersonalised, and becomes disconnected in a critical way from its core goals of reducing risks and impacts of disasters while improving lives and livelihoods. In conjunction with these developments, and increasing reliance and focus on using ‘Big Data’ to unlock some of the public health challenges of the modern world can lead to the use of cognitive heuristics that can lead to both blindness to scale and empathy loss. Though there is little doubt that a more strategic and purposeful interrogation of complex, large datasets may result in fresh insights to deliver the core goals of DRR, this is but one of many tools available to disaster and health managers. The associated risk is that large numbers and datasets can be dehumanising, and disaster management and health professionals need to be sensitised to this13.
The ethos and protocols offered by Schwartz Rounds offers an opportunity to reduce an increased risk of dehumanisation and empathy loss that a focus on global scale frameworks, or international/national/regional datasets might bring. In healthcare settings it has not been unusual for a false dichotomy to be set-up: that once must choose between compassionate or competent care, assuming that you cannot have both. The evidence indicates that this is untrue14. Organisations that focus on delivering compassionate care benefit from lower staff turnover, higher retention, recruitment of more highly qualified staff, and better health outcomes. Moreover, caregivers who are able to express compassion for patients, families, and each other experience higher job satisfaction, less stress and a greater sense of teamwork. A similar set of processes supported by careful facilitation that enable disaster managers and their interdisciplinary colleagues to regularly discuss the social and emotional dimensions of their work in an open and honest manner may help to deliver similar benefits in disaster management settings. Staff can be provided with an opportunity to share their experiences, thoughts and feelings on thought-proving subjects drawn from real-life disaster response and recovery cases. The critical premise is that staff are better able to make personal connections with their colleagues and those they are trying to assist when they have greater insight into their own responses and feelings. In this way, Schwartz Rounds or similar processes can decrease feelings of stress and isolation, and increase openness to giving and receiving support.
A focus on the impact of the human scale and impact of working in disaster management, whether in a health context or more broadly, can help to increase the sense that staff feel supported in their work, and can still be in touch with their empathic concern when working in difficult contents – from active disaster response to working to deliver actions determined by international agreements. In this way, we can help and support our most valued resource – our skilled workforce – to deliver effective, competent, and compassionate disaster management.
— Māori proverbHe aha te mea nui o te ao
What is the most important thing in the world?
He tangata, he tangata, he tangata
It is the people, it is the people, it is the people.
The workshop on the "Application of New Technologies in Disaster Management Simulation" was held in Tehran in January 2015. It was co-organized by the Disaster and Emergency Health Academy of Tehran University of Medical Sciences and Emergency and the Research Center in Disaster Medicine and Computer Science applied to Medicine (CRIMEDIM), Università del Piemonte Orientale. Different simulators were used by the participants, who were from the health system and other relevant fields, both inside and outside Iran.
As a result of the workshop, all the concerned stakeholders are called on to support this new initiative of incorporating virtual training and exercise simulation in the field of disaster medicine, so that its professionals are endowed with field-based and practical skills in Iran and elsewhere.
Virtual simulation technology is recommended to be used in education of disaster management. This requires capacity building of instructors, and provision of technologies. International collaboration can facilitate this process. Keywords: Virtual simulation, disaster management, education, training, Iran
]]>Introduction
The Islamic Republic of Iran (I.R.Iran) has been always exposed to disasters. The 2003 Bam earthquake accelerated the impetus of formulating effective disaster response and risk management actions in the whole disaster management and health systems of Iran.1,2 This revolution was supported by different stakeholders including government and academia. Thereafter, consistent with new strategies on disaster management, the necessity of relevant training initiatives was considered, in which the Master of Public Health (MPH) with disaster concentration, and the PhD program of Disaster and Emergency Health were developed in Iran.3 Although this initiative consists of academic and field approaches, in respect to training and exercise interventions, there is high demand to import new educational technologies, with the aid of virtual training and simulation in the subject of disaster management. To fulfill this goal, the first workshop on “Application of New Technologies in Disaster Management Simulation” was organized by the Disaster and Emergency Health Academy of Tehran University of Medical Sciences (TUMS) in collaboration with the Research Center in Emergency and Disaster Medicine and Computer Science applied to Medicine (CRIMEDIM), Università del Piemonte Orientale, Italy.
Virtual simulation
In the past two decades, simulation has been used increasingly as part of the ongoing evolution of technology. Disaster medicine is among the fields where different simulation models have been integrated. The term “Simulator”, in relation to healthcare, refers to a device that presents a simulated environment, patient, and situations, and then interacts appropriately with the actions taken by simulation participant.4 Although the history of simulation techniques predates information technology, using computerized simulators has brought huge capabilities in producing a life-like world for instructors and trainees.5 The Society for Academic Emergency Medicine Simulation Task Force, established in 2005, has been keen to promote virtual simulation awareness and its incorporation in emergency medicine and healthcare.6 Such training provides students and researchers with opportunities to apply their medical theoretical knowledge in a safe and realistic setting, develop team working skills, and a systematic approach to problem solving.7 In this way, disaster medicine is a subject with a high potential to use computerized simulations tools and methods. In fact, due to ethical, logistic, and financial barriers, it is not easy to make a real simulated disaster situation for educational purposes. For instance, it is impossible to simulate a huge catastrophe like the Bam earthquake in training and exercise programs other than through computer simulation.
Within the past few years, there have been ongoing improvements in disaster exercises and simulations in the health system of Iran, but computerized simulation-related training benefits are yet to be appropriately realized and applied.
First workshop on application of new technologies in disaster management simulation in Iran
From 3rd to 6th January 2015, the TUMS in collaboration with CRIMEDIM organized a training workshop on application of new technologies in disaster management simulation in Tehran. It attracted participants studying and working in the health disaster arena. The training aim was fourfold to:
This four-day intensive program covered the following topics: incident scene management, triage and rescue operations; medical management of Chemical, Biological, Radiological and Nuclear (CBRN); management of medical systems and resources in pre-hospital and hospital operations; and evaluation of emergency exercises.
Aside from the presentations, with aid of the XVR Simulator® and ISEE Simulator® (E-Semble, Delft, The Netherlands)4, the trainers engaged participants in group based and tabletop computerized simulative exercises. These exercises mimic some mass causality incident (MCI) scenarios according to the training topics on triage and medical resource management, both in the pre-hospital and hospital setting. The simulation-based learning environment was created in accordance with the four criteria for designing effective simulations for learning procedural skills.8 At the end of the computerized exercises, structured debriefings were delivered based on the theoretical principles developed by Fanning and colleagues9, showing the objective data (i.e.: pre-hospital, in-hospital, dispatch center performance indicators10 and triage accuracy) easily gathered and presented with the use of the Disaster Simulation Suite – DSS® software (iNovaria, Novara, Italy).
As well as these commercial software, different free software was also demonstrated and used by participants, with the aim of training and exercise; for instance, TIER Threat Identification tool, TIER Risk Calculator, Electronic Mass Causality Assessment and Planning Scenarios (EMCAPS), and Virtual Community Reception Center (VCRC).11
At the workshop closure, almost all the participants’ evaluation comments called for more similar virtual simulation training opportunities across Iran given the mesmerizing and inspiring knowledge, skills and concepts they gained. For other participants, it was an opportunity to rehearse and identify their personal and institutional strengths and weaknesses in relation to their previous roles in some MCIs in Iran and elsewhere.
A need to incorporate virtual simulation in disaster education in Iran
The unpredictable and multifaceted exposure of the I.R.Iran to disasters warrants an urgent effort to endow disaster scholars and professionals with more practical skills rather than theoretical ones. Ideally, this can be fostered by exploiting virtual simulation training. With the recent initiative of the TUMS to organize training on new technologies in disaster management simulation, it is evident that adoption of virtual simulation in Iran is at hand. As a first step, this can be done most effectively by: conducting numerous and rapid countrywide consultations with various disaster professionals in order to identify the potential learners; assess their general and specific simulation educational needs; define learning objectives; and select the best teaching and training strategy for achieving each objective.5 The experience gained from this assessment can guide the development of a comprehensive virtual simulation teaching and learning approach and later be incorporated into the Iranian professional and academic training curricula.
Conclusion
With reflection on this assessment of the application of new technologies in disaster management simulation training in mind, we conclude by calling for support and extended collaboration within and outside Iran from all concerned to effectively incorporate virtual simulation with the ultimate goal of endowing disaster professionals with field-based and practical skills in Iran. The same call should also be made beyond Iran to other countries and regions known to be embroiled in devastating disasters.
Competing Interest
Ali Ardalan, Joseph Kimuli Balikuddembe, and Ali Akbarisari have declared that no competing interests exist. Pier Luigi Ingrassia, Luca Carenzo, Francesco Della Corte, and Ahmadreza Djalali are working for CRIMEDIM. Pier Luigi Ingrassia, Luca Carenzo, and Francesco Della Corte, partially own iNovaria (Novara, Italy), the academic spinoff company of the Universita` degli Studi del Piemonte Orientale ‘A. Avogadro’, and the DSS software. iNovaria is the sales partner of E-Semble Company (Delft, the Netherlands), the owner of the XVR and ISEE software.
Corresponding author
Ali Ardalan MD, PhD. Tehran University of Medical Sciences, Tehran, Iran; Harvard Humanitarian Initiative, Harvard University, Cambridge, USA. Email: [email protected]
Introduction
The previous three parts in this series demonstrate that Twitter has the potential to be an effective and efficient community-based communications tool for disaster risk reduction and management.1–3 The skills required for people to utilize Twitter effectively during a disaster or public health emergency range from effective tweet-based communication, including modifiers and hashtags, computer programming, health informatics, and statistical analysis.1–3 Some applications of this tool lie within the nascent domain of public health informatics. This tool, if properly harnessed, can aid public health providers in disaster risk reduction and management. Within the context of dynamic innovations in global communication and technology, public health education must evolve and adapt to meet the needs of the population that public health officials serve. This must be accomplished while effectively and efficiently staying true to the competencies and standards defined by the public health community as displayed with the “10 Essential Public Health Services.”4 Twitter and its informatics base has the potential to be integrated across disciplines and within all levels of public health infrastructure and social protection programs
Concepts
COMMUNITY ENGAGEMENT FOR DISASTER PLANNING AND MITIGATION
Twenty-first century public health workers and emergency managers need to be able to communicate with their communities in order to achieve resiliency. Social media now plays an ever greater role in communicating with populations in all phases of the disaster cycle: prevention, preparedness, response, and recovery. These studies demonstrate that for all disaster planning phases, public health workers and emergency management teams should initially focus on identifying and recruiting social media savvy individuals that have large followers in the local region or among the targeted and potentially at-risk population in building ‘disaster response follower’ bases. Using data from the 2013 Hattiesburg F4 tornado, user followers along with the Klout score were shown to be the strongest pre-storm significant indicators associated with exponential message distribution, allowing for the social media community leaders or superspreaders to be identified while allowing them to remain anonymous.1–3
This ability to identify community leaders enables public health officials and disaster managers to facilitate partnerships through recruitment and mobilization efforts within the community. The average Twitter follower has 208 followers, but local superspreaders, as demonstrated in Parts I-III, show the top 100 rated users have an average of 1,000 Twitter followers which is 5 times the average follower.1–3 If superspreaders (or community leaders) are provided proper competency-based training, this process has the potential for rapid and effective dissemination of information to a targeted population group via disaster and public health officials. Additionally, increasing the followers for superspreaders, community leaders, disaster response teams, and public health officials that use Twitter would allow for enhanced education, information dissemination, and empowerment of population groups previously inaccessible prior to the influence of social media. Past studies found that social media is changing current communication patterns.5 Community leaders and disaster managers, by engaging with these new social media communication tools have the potential to improve health outcomes by optimizing communication within each disaster phase.6 To date, a working relationship with social media and the tools it offers has not been a priority in the emergency management profession.
Burkle and Greenough emphasize the need for continued community engagement throughout the disaster cycle and the inherent challenges of monitoring public health outcomes in a crisis environment.7 The impact of compromised public health infrastructure and systems on health consequences defines and greatly influences the manner in which disaster are observed, planned for, and managed, especially those that are geographically widespread, population dense, and prolonged. What may first result in direct injuries and deaths may rapidly change to excess indirect morbidity and mortality as essential public health resources are destroyed, deteriorate, or are systematically denied to vulnerable populations.”7 Community engagement with Twitter can greatly enhance the immediate situational awareness leading to a more directed response and recovery actions. The “prepared community concept” popular in Australia has led to more “effective and efficient” response and recovery phases of the disaster cycle.8
COMMUNITY ENGAGEMENT FOR DISASTER RESPONSE AND RECOVERY
Disaster notification resources must adapt and evolve to the reality that the at-risk populations may not have access to local television, radio, or be within range of warning sirens during a disaster. This confirms the need for practical applications of social media assets. Currently, much of the social media research in the realm of public health is placed on the academic perspective of investigation where the emphasis is focused on proving an application’s worth in controlled environments or groups. This limits the practical application, even for trained public health and disaster managers, as the application must be broadened to allow for the targeting of a population group while accounting for behaviors unique to that population. In this series, Twitter has shown unique features with the potential to be utilized for practical application by disaster officials and public health managers across and within the disaster cycle.1–3
Parts I-III highlight the features of Twitter that allow for it to be effectively utilized by disaster and public health managers as a publicly accessible and cost-effective network for instantaneous dissemination. Additional features include the ability to collect accurate and reliable data both retrospectively and in real-time, and the capacity to target a population group, all while allowing those who use it to maintain anonymity. These qualities allow for an easy and practical application in all phases of disaster management but call for additional education, training and program development before any application of this technology in monitoring and health surveillance can be effectively operationalized.
COMPETENCY BASED EDUCATION AND TRAINING
Current education and training programs for the public health workforce for the 21st century do not necessarily prioritize the competencies and skills that are required to best utilize technology and social media interventions including Twitter. The Core Competencies for Public Health Professionals (Core Competencies) are defined by skill sets for broad practice of public health defined by “10 Essential Public Health Services”.4,9 These provide a framework for National Public Health Performance Standards (NPHPS) and public health educators.10 The competencies for public health professionals are developed by the Council on Linkages Between Academia and Public Health Practice (Council on Linkages), which is funded by the Centers for Disease Control and Prevention (CDC) and is supported by the Public Health Foundation consisting of a collaboration of 20 national organizations. They are designed to improve public health education, training, research, and workforce development through evidence-based practice of public health.11 These competencies are dynamic and constantly evolving to meet the needs of the public health field and the population groups the health providers serve.12 Yet, the current competencies are limited in providing direction and standards on communication within technology and social media, such as Twitter. If competencies are provided to the public health community, the proper infrastructure, training, and policy can be developed to harness the potential of this global communication tool through technology while a public health alliance works to instill standards to ensure proper ethical, legal and transparent applications as the technology evolves in the future.
Past studies proposed that disaster-specific public health preparedness competencies should place greater value on the use of social media skills for relevant risk communication.13,14 However, these studies do not fully appreciate the requirements for competency for global adaptation of this tool within an ever-changing multidimensional technological environment across the world. For operational application of social media, performance competency is vital to permit ethical and sustainable implementation of technology. It would allow for it to be taught at all levels and fields of public health. Standards would progress the field of public health in the age of technology while aiding in efficiently carrying out the basic public health functions of assessment, policy development, and assurance. Additionally, this would allow for cross-disciplinary and multidisciplinary adoption of standards.
Domain: Public Health and Disaster Informatics Competency Recommendations Include:
1) Ethical and effective communications using Twitter and other social media outlets during all phases of the disaster life cycle.
2) Effectively modify tweets and social media messages to positively enhance dissemination of information with cross-cultural competency to meet the needs of a target population group, allowing for better information, education, and empowerment of the population group across the disaster life cycle.
3) Effectively program data sets to filter and triangulate data for a targeted population during all phases of the disaster life cycle.
4) Facilitate the use of technology and social media, such as Twitter, to aid in community mobilization and partnerships to identify and solve health problems during all phases of the disaster life cycle.
5) Apply appropriate statistical analyses and data retrieval techniques to allow for accurate and reliable data recovery during all phases of the disaster life cycle.
6) Ethically monitor, investigate, and survey health problems and hazards with real-time surveillance systems and databases leveraging Twitter and other social media outlets during all phases of the disaster life cycle.
7) Ensure competency-trained access of technology and social media outlets such as Twitter for all levels of disaster managers and public health providers during all phases of the disaster life cycle.
8) Emphasize the importance of translating academic research to practical public health application during all phases of the disaster life cycle.
9) Develop and evolve ethical policies, laws, and regulations to protect health and ensure safety of all who use technology and social media such as Twitter during all phases of the disaster life cycle.
10) Evaluate and monitor the effectiveness, accessibility, and quality of population-based health information obtained through technology and social media such as Twitter during all phases of the disaster life cycle.
11) Apply transparency, systemic, consistent, comprehensive, accurate, and reliable data collection methods from social media, such as twitter, for assessment, development, implementation, evaluation, and reassessment/modification of public health programs and initiatives during all phases of the disaster life cycle.
Communication is fundamental to public health.14 These competencies must be embedded in public health schools and become part of the foundation for today’s evolving public health education and disaster management. Public health schools should take the lead in training future public health and disaster managers to acquire these skill sets to meet the needs of the population they serve. Program managers are expected to consistently target and meet their population group needs while promoting initiatives allowing for cost efficiency and maintaining integrity of the public health program; and allow for adoption of those needs both with direct interest while sharing technological advances with others in the field.15,16 For these expectations to occur, new skill sets must evolve along with technology.
EDUCATION AND TRAINING TO PROMOTE RESILIENCY
For implementation and sustainability of this technology in the field of public health and disaster management funding must be provided at all levels. Funding would allow for training and education in public health schools linked to communities to meet these competency requirements. Funding for state and local public health must be provided for real-time monitoring, disease surveillance, program monitoring and evaluation, and for training and education of public health workers and emergency managers responsible for disaster planning in their communities. Additionally, funding would be required for readiness assessment exercises to assess training and monitor standards.11,13 Each would allow for communities to be prepared for potential threats while implementing the most up-to-date efficient tools. Due to the unique criteria required for disaster response the CDC plays a key role in ensuring state and local agencies are prepared for disaster preparedness and are the main source of funding from the Public Health Emergency Preparedness cooperative agreement. Unfortunately, this funding is declining.17 In light of this decrease it becomes crucial to prioritize funding for the development of a sustainable infrastructure, especially at the local level, which might leverage the greater efficiency and cost-effectiveness provided by social media.
Limitations
Competency-based content has its limitations. There are different ways in which one improves their skills: through practice of those skills, through professional development to practice in a competent manner, and to properly identify indicators by which their practice may be recognized as having achieved certain levels of proficiency. Twitter users come to this task in disaster risk reduction with daily experience in its usage. This project speaks only of honing that development in terms of expectations around a specific disaster event. There remains a paucity of experience other than what is described in this study. The competencies listed represent guidance the authors consider today as core requirements. Competencies will change as the technology improves, as Twitter is used in a variety of disaster and crisis events, as the practice environment evolves, and as professional standards and legal regulations of practice are determined. The competencies presented here provide a general framework that should allow for the launching of the structured education and training to progress.
Conclusions
Twitter, if properly harnessed, can aid public health providers in providing low cost and effective disaster risk reduction and management. This process has the potential of meeting all the basic public health functions of assessment, policy development, and assurance. It is also likely that the above competencies may be broadened for daily public health functions and tasks. Planners must not lose sight that this process should be accomplished as part of community planning especially in disaster-prone communities and regions worldwide. The evidence provided by these studies originated from a disaster prone area in Mississippi, yet demonstrates the first steps of what can be accomplished on a wider scale.
Competing Interests
The authors have declared that no competing interests exist.