Abstract
Introduction: During the flare-ups of Ebola virus disease (EVD) in Liberia, Sinoe County reactivated the multi-sectorial EVD control strategy in order to be ready to respond to the eventual reintroduction of cases. This paper describes the impacts of the interventions implemented in Sinoe County during the last flare-up in Monrovia, from April 1 to June 9, 2016, using the resources provided during the original outbreak that ended a year ago.
Methods: We conducted a descriptive study to describe the key interventions implemented in Sinoe County, the capacity available, the implications for the reactivation of the multi-sectoral EVD control strategy, and the results of the same. We also conducted a cross-sectional study to analyze the impact of the interventions on the surveillance and on infection prevention and control (IPC).
Results: The attrition of the staff trained during the original outbreak was low, and most of the supplies, equipment, and infrastructure from the original outbreak remained available. With an additional USD 1755, improvements were observed in the IPC indicators of triage, which increased from a mean of 60% at the first assessment to 77% (P=0.002). Additionally, personnel/staff training improved from 78% to 89% (P=0.04). The percentage of EVD death alerts per expected deaths investigated increased from 26% to 63% (P<0.0001).
Discussion: The low attrition of the trained staff and the availability of most supplies, equipment, and infrastructure made the reactivation of the multi-sectoral EVD control strategy fast and affordable. The improvement of the EVD surveillance was possibly affected by the community engagement activities, awareness and mentoring of the health workers, and improved availability of clinicians in the facilities during the flare-up. The community engagement may contribute to the report of community-based events, specifically community deaths. The mentoring of the staff during the supportive supervisions also contributed to improve the IPC indicators.
Funding Statement
The authors received no specific funding for this work.Introduction
The Ebola virus disease (EVD) outbreak started in Guinea in 20131,2, and as of June 10, 2016, 28,616 cases had been registered, with 11,310 deaths32. After the end of the original outbreak, in the three most affected countries in 20152, specifically, in Liberia in May, Sierra Leone in November, and Guinea in December, different flare-ups were reported. The biggest flare-up was in Guinea, which occurred from February 274 to June 1, 2016, with 10 reported cases and seven deaths3, while the smallest one was in Sierra Leone, from January 14 to March 17, 2016, with two reported cases and one death5.
Flare-ups may occur due to importation, reintroduction of the virus from an animal reservoir, a missed chain of transmission, or reemergence of the virus from a survivor4,6,7,8,9,10, and can be easily detected when EVD surveillance, including community-based surveillance and laboratory capacity, is established11. EVD flare-ups can also be controlled on time when a multi-sectorial EVD control strategy is implemented effectively. This strategy involves different committees, including clinical case management, surveillance, laboratory, logistic, behavioral and social interventions, psychosocial support, coordination, and others11.
Liberia reported three flare-ups after the initial declaration of “disease-free” status on May 9, 20152,12,13, the first one being from June 29 to September 3, 2015 in Margibi County14, which occurred after the re-emergence of the virus from a survivor through sexual contact12,14, and the second one being in Duport road, Monrovia, from November 24, 201515,16 to January 14, 2016, which started from a pregnant Ebola survivor who became infectious when her immune system weakened due to the pregnancy15. The two flare-ups were detected through a postmortem swab tested for EVD14,15. The last flare-up, which occurred from April 1 to June 9, 2016, was imported from Guinea3. All the flare-ups were detected early, during the 90 days of enhanced EVD surveillance recommended after the end of the outbreak, which includes the swabbing of all dead bodies for EVD laboratory investigation17. The active Incident Management System (IMS) for coordination, a temporary field-based Emergency Operation Center (EOC), implementation of the rapid response plan developed to respond to eventual flare-ups, and the presence of experienced staff trained during the original outbreak contributed to early containment of the flare-ups14.
Sinoe County reported 22 confirmed EVD cases and 11 deaths during the original outbreak, which was controlled with the isolation of the cases18, establishment of Ebola task forces, training of the staff, and other strategies19,20.The last confirmed case died in December 2014 and no flare-up was reported in the county. However, during the flare-ups in Liberia and neighboring countries, Sinoe County reactivated the multi-sectorial EVD control strategy in order to be ready to respond to the eventual reintroduction of cases.
This paper describes the impacts of the interventions implemented in Sinoe County during the last flare-up in Monrovia, using the resources provided during the original outbreak, in order to be ready to respond to the eventual importation of cases.
Methods
Setting
Sinoe County, one of the southeastern counties in rural Liberia, is divided into 10 health districts, four of which have a history of EVD positive cases reported during the original outbreak (Fig. 1)21, and 305 communities. The capital city, Greenville, is located at about 150 miles from the capital of Liberia, Monrovia. The population is dispersed, with 104,932 inhabitants and a density of 27 people per square mile22. It is difficult to reach many communities on account of forests, rivers, swamps, and hills, and the average distance from community to healthcare facility is 6.6 km21,23. However, in each of the communities, there is a community health volunteer who is responsible to provide voluntary health services such as referrals, health awareness, treatment of simple malaria, diarrhea, common cold, and pneumonia in children within the age range of 2months to 5 years. During the original outbreak, when Sinoe County reported confirmed cases of EVD, 250 of the community volunteers were trained in contact tracing and deployed immediately in communities with contacts, including Poly town community where they detected a secondary chain of transmission. The county is also served by two medical doctors, 18 physician assistants, and 67 nurses, and it has 35 health facilities, including one referral hospital with a capacity of 100 beds, and 34 clinics21.
Fig. 1: Map of Sinoe County, Liberia, showing the number of Ebola virus disease cases reported per district during the original outbreak in 2014.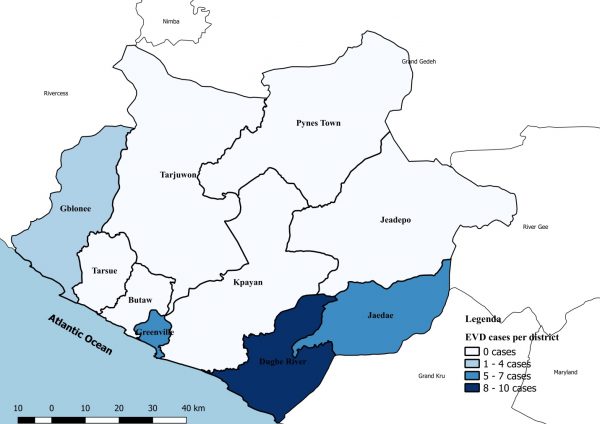
Study design
We conducted a descriptive study to describe the key interventions implemented in the county from April 1 to June 9, 2016, the capacity available, the implications for the reactivation of the multi-sectoral EVD control strategy, and the results of the same. We also conducted a cross-sectional study to analyze the impact of the interventions on surveillance and infection, prevention, and control (IPC).
Data analysis
We entered the data into MicrosoftTM Excel and used MedCalc® Statistical Software version 17.224 for IPC and EVD surveillance data analysis. To determine statistical significance, we performed Student’s t-test for the IPC assessment data and the chi-squared test for the EVD surveillance data. We calculated the number of expected deaths using the crude death rate in Liberia, of 8.8 deaths/1000 population/year25,26.
Key interventions
We reactivated the different committees involved in the EVD control activities, as recommended by the WHO (Fig. 2)11.
Fig. 2: The organizational structure of the Ebola virus disease control activities highlighting the committee activated in Sinoe County, Liberia, during the flare-up of 2016.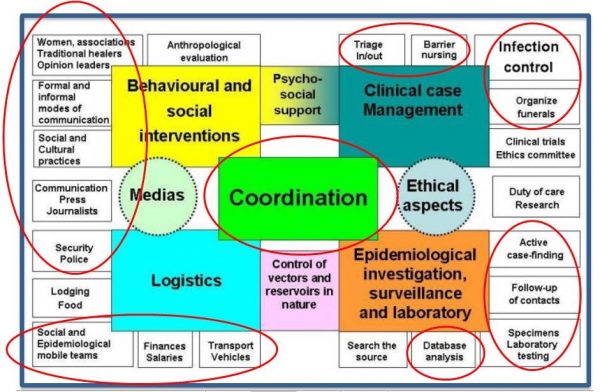
Coordination
The county health team (CHT) developed an emergency plan to prepare for responding to the eventual importation of cases from Monrovia using the resources provided during the original outbreak. When the end of the flare-up was declared, we analyzed the level of implementation of the plan as well as the costs involved.
The coordination committee conducted meetings with county, district, and community stakeholders, partners, and other line ministries for coordination, awareness, and advocacy, in order to mobilize resources.
Logistics, human resources and, Infection Prevention and Control assessments
We analyzed the human resources database to assess how many Rapid Response Team (RRT) members, contact tracers, and burial team members trained during the original outbreak were available in the county during the last flare-up.
Using the minimum standards assessment tool developed during the original outbreak (Appendix: S1 File), we conducted the first integrated assessment of the logistic capacity available at 30 (88%) health facilities in the county, including the referral hospital, in April 2016. However, five (14%) of the 35 health facilities in county were inaccessible.
After the initial assessment we replenished the supplies, mentored the health care workers, and conducted the second assessment from the end of May to October, 2016 to verify the changes. The assessments were conducted through direct observation, interviews of the healthcare workers, and perusal of the documents available (Appendix: S1 File).
We also assessed the 10 most important check points connecting Sinoe County and other counties to verify the knowledge of the staff and availability of IPC supplies.
Clinical case investigation, surveillance, and laboratory
We conducted supportive supervisions at 30 (88%) health facilities in Sinoe County and held weekly meetings with district health officers and district surveillance officers to reinforce the triage of all the patients, the use of the EVD outbreak case definitions, and to analyze the EVD surveillance situation in the county. Besides using the WHO case definition for the investigation of cases (Fig. 3)27 we collected swabs of all the dead bodies, regardless of the cause of death, to perform real-time quantitative reverse transcription PCR (qRT-PCR) before and during the flare-up, as part of the 90 days of enhanced surveillance implemented after the end of each EVD outbreak.
Fig. 3: The World Health Organization’s case definition of Ebola virus disease used during the outbreaks and used in Sinoe County before and during the flare-up in Liberia, from April to June 2016.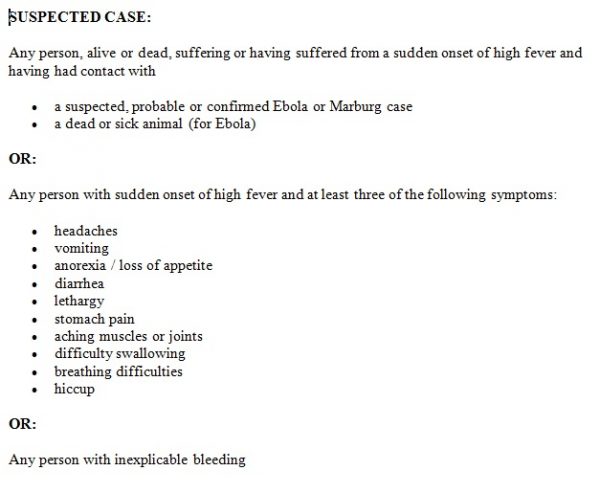
The specimens were collected by trained clinicians and lab staff in all the health facilities in the county and were transported to the regional labs in Liberia with the capacity to perform the qRT-PCR for EVD. We perused all the lab records to quantify the numbers of specimens collected before and during the flare-up.
Contact Tracing
We conducted a rapid assessment of availability of contact listing, follow-up, reporting and monitoring forms, as well as the availability of staff with experience in contact tracing supervision. The partners were mobilized to provide logistic support for contact tracers and supervisors as well as food and water for the contacts.
Behavioral and social interventions
We disseminated EVD prevention messages through radio talk shows with county authorities and traditional leaders at a local radio station. We also conducted community meetings in high-risk communities, churches, mosques, and funeral and healing homes to increase awareness and to encourage the reporting of community deaths to the health facilities.
Ethical considerations
Ethical approval was not required to implement the activities, as they were part of the public health interventions of the Ministry of Health to respond to outbreaks in Liberia. We did not use any confidential data and did not disclose any unauthorized names in our report.
Results
Coordination
The county’s task force for EVD was activated and was responsible to ensure that the preventive measures were implemented at all levels and that any suspected case was promptly reported. As the resources were already available from the original outbreak, the three-month plan cost an additional USD 1755 besides the budget for the routine activities. The dissemination of EVD prevention messages to churches, mosques, households, meetings in high-risk communities, and funeral and healing homes was the most expensive activity, at about USD 400. This was mostly attributable to purchasing fuel for the activities and paying daily subsistence allowance (DSA) for the staff (Table 1).
Table 1: List of the main activities implemented routinely and during the flare-up of Ebola virus disease prevention and surveillance in Sinoe County, Liberia, in 2016.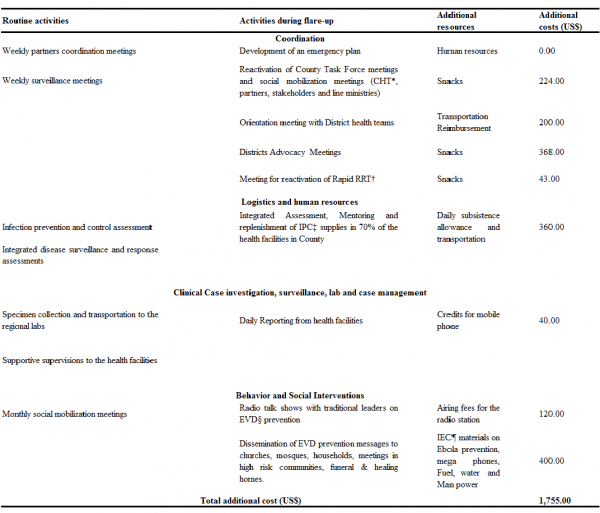
Logistics, human resources, and Infection Prevention and Control (IPC) assessments
At the first assessment, we included 30 health facilities (29 clinics and one hospital) in our analysis of the IPC indicators. From this analysis, we excluded the indicators that were not applicable to clinics (Appendix: S1 File), according to the tool used. Personnel/staff training was the group of indicators with the highest scores. The mean of the four individual indicators in this group was 78% [standard deviation (SD) = 11%] including 90% of the health facilities with staff trained in IPC by the Ministry of Health and Social Welfare (MOHSW) in a training called “keep safe keep serving.” Additionally, 63% had staff meeting the criteria outlined in the MOHSW’s Essential Package of Health Services (EPHS), the minimum skills required to work in the facilities (Table 2). On the other hand, the group of four indicators for triage had a mean of 60% (SD = 12%), and the other three indicators assessing the facilities in terms of having an appropriate isolation space ready to receive cases had a mean of 52% (SD = 9%). The structure of the community care center in the Karquekpo community, with a capacity of 12 beds, and the ETU in Greenville district, with a capacity of 60 beds, remained intact, but these facilities required equipment and supplies to start receiving patients. Out of the facilities assessed, 27 (90%) had IPC supplies that would last them for one month. These supplies were provided during the original outbreak.
Table 2: Performance of the Infection Prevention and Control indicators in Sinoe County at the beginning (baseline) and at end (reassessment) of the flare-up in Monrovia, Liberia, in 2016. *The mean percentage was calculated for each group of indicators; †P-value was calculated for each group of indicators using a paired t-test and was considered statistically significant when ≤ 0.05; ‡n = number of the health facilities where the indicator was assessed. In total, 17 health facilities (n = 17) were assessed and reassessed with the same tool, while 13 health facilities were reassessed with a new tool that excluded some indicators; §SD = standard deviation; it was calculated based on a sample for the group of indicators; ¶Indicator was not included in the new tool used for the reassessment of 13 clinics; **Indicator was not included in the new tool for reassessment but was assessed in two clinics where the tool was used.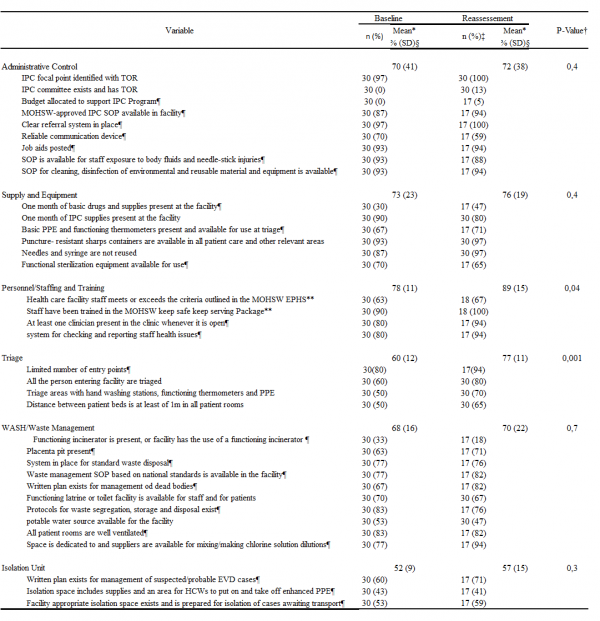
In the second assessment, significant improvements were observed on the indicators of triage (an increase from 60% during the first assessment to 77% on reassessment; P = 0.002) and personnel/staff training (an increase from 78% to 89%; P = 0.04), while other indicators did not exhibit significant improvements.
The lab supplies for the oral swab of dead bodies and whole blood for live alert investigation were available in all the facilities (100%) during the first and second assessments.
The county had three vehicles that were available to be used in case of an outbreak, including one ambulance for the transportation of cases.
Of the 21 members of the RRT trained during the original outbreak, 19 (90.5%) remained present in the county. All 250 (100%) community volunteers trained for contact tracing remained in their communities, and they were available to resume the task in case of need. Of the 14 members of the two burial teams trained during the previous outbreak, 12 (86%) remained present in the county.
All 10 most important checkpoints connecting Sinoe with other counties had a bucket for handwashing and thermometers, although some were not functional. After mentoring the staff and replacing the thermometers, nine (90%) check points reactivated the monitoring of temperature and handwashing for people crossing these locations.
Clinical case investigation, surveillance, and laboratory
The percentage of EVD death alerts investigated, including the oral swabs collected and sent to the regional lab in Liberia, increased from 26% of the death alerts per expected deaths during the three months before the flare-up in Monrovia, to 63% of the alerts per expected deaths during the flare-up (P < 0.0001). Significant improvement was verified in seven of the 10 health districts in the county. On the other hand, the number of live alerts investigated and the whole blood tested for EVD decreased from 0.5 alerts per 100 population to 0.4 alerts per 100 population (P = 0.0003). The reduction was significant in Greenville (P < 0.0001) and Butaw (P = 0.05) districts (Table 3). All the specimens from both live and death alerts came negative for EVD. The total number of health facilities investigating death alerts increased from 19 (Mean = 54% per health district, SD = 34%) to 28 (Mean = 83% per health district, SD = 22%) health facilities (P = 0.006) in all 10 health districts in the county (Fig. 4).
Contact tracing
All the reporting and monitoring tools used during the original outbreak were available and would be reproduced according to number of eventual contacts listed. All the county supervisors and partners, including World Health Organization (WHO) had experiences from the original outbreak. In case of eventual importation of cases, the county surveillance officer, the county monitoring and evaluation officer and the epidemiologists from WHO present in County would be in charge of contact listing as well as to provide one day orientations to the experienced community volunteers responsible for home visits to the contacts. All the 10 district health officers (DHOs) present in county also had experiences from the previous outbreak and would support the supervision of contact tracers together with county supervisors and partners. There was no formal commitment from the local partners to provide incentives for contact tracers and supervisors as well as food and water for contacts. The IPC materials and thermometers in stock in county would be used also for contact tracing in case of need.
Table 3: Live and death alerts investigated in Sinoe County before and during the flare-up in Monrovia, Liberia, in 2016. *P-value was calculated using the chi-squared test for comparing two proportions; it was considered statistically significant when ≤ 0.05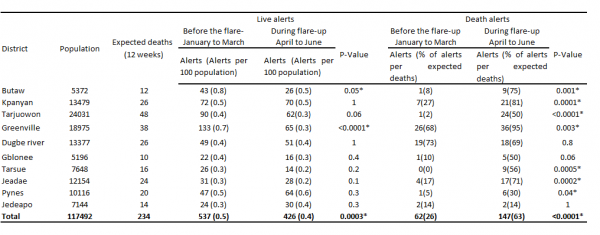
Fig. 4: Percentage of healthcare facilities investigating Ebola virus disease alerts in Sinoe County three months before and during the flare-up in Monrovia, Liberia, in 2016. The error bars show the standard deviations (SD) for the percentage of health facilities per health district (total = 10 health districts) investigating at least one alert from January to March and from April to June, 2016. P = 0.3 for live alerts and P = 0.006 for death alerts in Sinoe County, Liberia, calculated using the chi-squared test for comparing two proportions; P was considered statistically significant when ≤ 0.05. N = 34 health facilities in Sinoe County.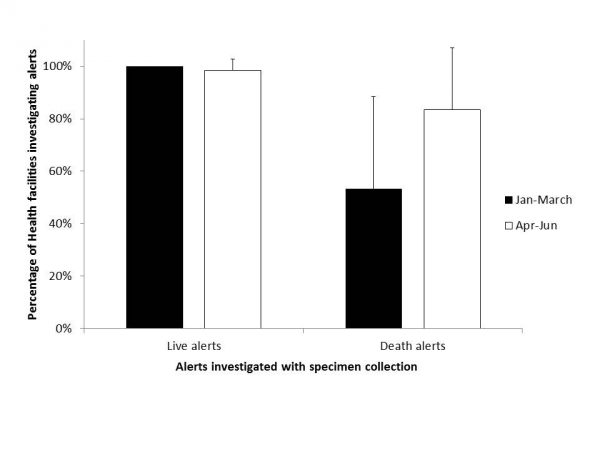
Discussion
The interventions implemented in Sinoe County in preparation to respond to the reintroduction of EVD cases from the last flare-up in Monrovia had a significant impact on EVD surveillance, leading to an increase in percentage of death alerts from 26% alerts per expected deaths during the three months before to 63% alerts per expected deaths during the flare-up (P < 0.0001). This finding may have been affected by community engagement activities, awareness and mentoring of the health workers, and improved availability of clinicians in the facilities during the flare-up. Similar findings were reported in Lofa County, Liberia, during the original outbreak in 2014, when more community deaths were reported to the health authorities to be investigated for EVD after community sensitization and acceptance28. The reasons for reduction of live alerts were not clear from our study, and the same may have occurred owing to the increased attention focused on the death alerts during the flare-up, considering that the reporting and investigation of live alerts was already high in the county before the flare-up.
The improvements on the indicators of triage (from 60% at the first assessment to 77% on reassessment; P = 0.002) suggest that the mentoring of the staff during the first assessment led to behavioral change among health workers, leading to better triaging for EVD when people visited the facility. The on-site training of the staff also improved the indicators pertaining to personnel/staff training from 78% to 89% (P = 0.04), as these indicators do not require any interventions other than on-site mentoring. The mentoring of the staff also contributed to an improvement in the system for checking and reporting staff health issues in the facilities, and led to the permanent presence of trained clinicians whenever the facility was open. However, no significant improvement was verified in other indicators like equipment and infrastructure for isolation units, which require interventions from higher administration levels, as the procurement of supplies and construction of infrastructure may be slow because the county is not currently reporting any EVD-positive cases. A similar assessment conducted in Sierra Leone in 2014 led to a quick intervention from stakeholders and partners evidenced by the immediate provision of equipment and supplies, considering that, unlike Sinoe County in Liberia, these districts were facing an active EVD outbreak29.
The presence of trained staff in 90% of the health facilities; the small attrition of RRT members, contact tracers, and trained burial team members trained during the original outbreak; the availability of stock of IPC supplies for at least one month in 27 (90%) facilities; and other logistics, including the availability of three vehicles, rendered the reactivation of the multi-sectoral EVD control strategy fast and relatively affordable. In addition, despite the lack of supplies to attain full functionality, the presence of an isolation space for receiving patients in 43% of the health facilities, and the presence of an ETU with a capacity of 60 beds and a CCC with a capacity of 12 beds suggest that few additional interventions would be required to respond to any eventual importation of cases from Monrovia or elsewhere.
Our study has several potential limitations. First, the assessments were conducted as emergency interventions, and not enough time was available to train the personnel who conducted these assessments. However, the personnel received orientations during a two-hour meeting conducted before the assessment. In addition, a new improved tool for reassessment was introduced before the end of the flare-up. Therefore, two different tools were used for assessment and reassessment, although some indicators did not change. Thus, only 17 (49%) facilities were assessed and re-assessed using the same tool. To minimize this limitation, our analysis only included the indicators present in both tools. The time interval from assessment to reassessment was not the same for all health facilities, varying from one to five months. Thus, some facilities may have had more time to improve than others did.
Additionally, there may have been an information bias due to fatigue of the interviewed staff, as the facilities were receiving more visitors than usual during the flare-up. This may have led them to provide answers that would not require follow-up questions. Further, the interventions were implemented when the county did not report any confirmed EVD cases. Thus, some key areas of EVD response, like access to food and other supplies by contacts during contact tracing and case management, were not assessed. Our study did not determine if the supplies provided and the staff trained would remain available in the county if a flare-up occurred two or more years after the end of the original outbreak, nor did it assess the implications of this. Despite these potential limitations, our findings may be considered for assessing the preparedness for EVD and other future outbreaks, leading to improved surveillance, early detection, and control, as well as prevention of infection among health workers.
In conclusion, as part of outbreak preparedness, community engagement may contribute to the reporting of community-based events, specifically community deaths for EVD surveillance. The mentoring of the staff at health facilities, combined with the assessment of IPC, would lead to behavioral change among the health workers, thereby increasing IPC compliance and improving outbreak surveillance. The low attrition among the personnel trained in outbreak response, and presence of supplies at health facilities made easier, faster, and affordable to achieve the reactivation of the response structures.
We recommend a periodic reassessment of IPC supplies and equipment in health facilities, combined with mentoring of health workers, early advocacy for partners and stakeholders to provide the required equipment and to facilitate the construction of isolation units, and the implementation of reinforcement measures to reduce attrition among the trained health workers, especially within the first year after the end of any outbreak.
Data Availability
All data supporting this study are openly available from figshare, https://doi.org/10.6084/m9.figshare.4902929.
Competing Interests
The authors have declared that no competing interests exist.
Corresponding Author
Jeremias Naiene: [email protected]
Appendix
Acknowledgements
We thank Benjamim Karmo, Leleh Gornor-Pewu, Anthony Moore and Matirankie Kanneh for the support provided for the data analysis, social mobilization and assessments conducted in Sinoe County during the flare-up in Monrovia. We would also like to show our gratitude to Medical Teams International for orientations provided to the rapid response team in Sinoe County, United Nations International Children’s Emergency Fund for the technical support provided for social mobilization activities and Riders for Health for the specimens transportation to the regional laboratories.References
- Aylward B, Barboza P, Bawo L, Bertherat E, et al. Ebola virus disease in West Africa--the first 9 months of the epidemic and forward projections. N Engl J Med. 2014 Oct 16;371(16):1481-95. PubMed PMID:25244186.
- Shultz JM, Espinel Z, Espinola M, Rechkemmer A. Distinguishing epidemiological features of the 2013-2016 West Africa Ebola virus disease outbreak. Disaster Health. 2016;3(3):78-88. PubMed PMID:28229017.
- WHO. EBOLA SITUATION REPORT. World Health Organization. 2016;(10 JUNE):1–2
Reference Link - Diallo B, Sissoko D, Loman NJ, Bah HA, et al. Resurgence of Ebola Virus Disease in Guinea Linked to a Survivor With Virus Persistence in Seminal Fluid for More Than 500 Days. Clin Infect Dis. 2016 Nov 15;63(10):1353-1356. PubMed PMID:27585800.
- WHO. EBOLA SITUATION REPORT. World Heal Organ. 2016;(16 March)
Reference Link - WHO. EBOLA SITUATION REPORT. World Heal Organ. 2016;(20 January)
Reference Link - Geisbert TW. Persistence of Ebola virus RNA in seminal fluid. Lancet Glob Health. 2017 Jan;5(1):e12-e13. PubMed PMID:27955770.
- Fallah MP, Skrip LA, Dahn BT, Nyenswah TG, et al. Pregnancy outcomes in Liberian women who conceived after recovery from Ebola virus disease. Lancet Glob Health. 2016 Oct;4(10):e678-9. PubMed PMID:27633422.
- Mate SE, Kugelman JR, Nyenswah TG, Ladner JT, et al. Molecular Evidence of Sexual Transmission of Ebola Virus. N Engl J Med. 2015 Dec 17;373(25):2448-54. PubMed PMID:26465384.
- Abbate JL, Murall CL, Richner H, Althaus CL. Potential Impact of Sexual Transmission on Ebola Virus Epidemiology: Sierra Leone as a Case Study. PLoS Negl Trop Dis. 2016 May;10(5):e0004676. PubMed PMID:27135922.
- STRATEGY, EBOLA.Ebola and Marburg virus disease epidemics: preparedness, alert, control, and evaluation. (2014).
Reference Link - WHO. EBOLA SITUATION REPORT. World Health Organization. 2015;(15 July):1–16
Reference Link - Ministry of Health and Social Welfare. Liberia Ebola Daily Sitrep th no . 425 for 14 July 2015 : 2015;(425).
Reference Link - Bawo L, Fallah M, Kateh F, Nagbe T, et al. Elimination of Ebola Virus Transmission in Liberia - September 3, 2015. MMWR Morb Mortal Wkly Rep. 2015 Sep 11;64(35):979-80. PubMed PMID:26355323.
- Kaye D. Clinical Infectious Diseases 15 March News. Clin Infect Dis. 2015
Reference Link - MOHSW Liberia. Ebola Virus Disease Outbreak Response in Liberia : Information Bulletin-24 Nov 2015.
Reference Link - WHO. EBOLA SITUATION REPORT. World Heal Organ. 2016;2016(2 March)
Reference Link - MOHSW. Viral Hemorrhagic Fever Database. Sinoe County, Liberia; 2014
- Allen, Denise Roth Lacson, Romel Gblorie, Amos Patel, Manisha Beach M. Understanding Why Ebola Deaths Occur at Home in Urban Montserrado County , Liberia Report on the Findings from a Rapid Anthropological Assessment Table of Contents. 2015;(June)
Reference Link - Hagan JE, Smith W, Pillai SK, Yeoman K, et al. Implementation of Ebola case-finding using a village chieftaincy taskforce in a remote outbreak - Liberia, 2014. MMWR Morb Mortal Wkly Rep. 2015 Feb 27;64(7):183-5. PubMed PMID:25719680.
- Williams GS, Naiene J, Gayflor J, Malibiche T, Zoogley B, Frank WG Jr, Nayeri F. Twenty-one days of isolation: A prospective observational cohort study of an Ebola-exposed hot zone community in Liberia. J Infect. 2015 Aug;71(2):150-7. PubMed PMID:25982026.
- Johnson-sirleaf E. GOVERNMENT OF THE REPUBLIC OF LIBERIA 2008 NATIONAL POPULATION AND HOUSING CENSUS : PRELIMINARY RESULTS. 2008;(June)
Reference Link - MINISTRY OF HEALTH & SOCIAL WELFARE-Republic of Liberia. Country Situational Analysis Report. 2011;(July)
Reference Link - MedCalc Software bvba. MedCalc Statistical Software version 17.2. Ostend, Belgium; 2017
Reference Link - Global Health Observatory data repository. Crude birth and death rate Data by country. 2015.
Reference Link - The world bank. World development indicators, Death rate, crude (per 1,000 people). 2015.
Reference Link - World Health Organization. CONTACT TRACING DURING AN OUTBREAK OF EBOLA VIRUS DISEASE. 2014;(September)
Reference Link - Kouadio KI, Clement P, Bolongei J, Tamba A, et al. Epidemiological and Surveillance Response to Ebola Virus Disease Outbreak in Lofa County, Liberia (March-September, 2014); Lessons Learned. PLoS Curr. 2015 May 6;7. PubMed PMID:26064783.
- Pathmanathan I, O'Connor KA, Adams ML, Rao CY, Kilmarx PH, Park BJ, Mermin J, Kargbo B, Wurie AH, Clarke KR. Rapid assessment of Ebola infection prevention and control needs--six districts, Sierra Leone, October 2014. MMWR Morb Mortal Wkly Rep. 2014 Dec 12;63(49):1172-4. PubMed PMID:25503922.

Leave a Comment
You must be logged in to post a comment.