Abstract
AIM: The aim of this systematic literature review was to identify the extent and implications of medication loss and the burden of prescription refill on medical relief teams following extreme weather events and other natural hazards.
METHOD: The search strategy followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Key health journal databases (Medline, Embase, PsycINFO, Maternity and Infant Care, and Health Management Information Consortium (HMIC)) were searched via the OvidSP search engine. Search terms were identified by consulting MeSH terms. The inclusion criteria comprised articles published from January 2003 to August 2013, written in English and containing an abstract. The exclusion criteria included abstracts for conferences or dissertations, book chapters and articles written in a language other than English. A total of 70 articles which fulfilled the inclusion criteria were included in this systematic review.
RESULTS: All relevant information was collated regarding medication loss, prescription loss and refills, and medical aids loss which indicated a significant burden on the medical relief teams. Data also showed the difficulty in filling prescriptions due to lack of information from the evacuees. People with chronic conditions are most at risk when their medication is not available. This systematic review also showed that medical aids such as eye glasses, hearing aids as well as dental treatment are a high necessity among evacuees.
DISCUSSION: This systematic review revealed that a considerable number of patients lose their medication during evacuation, many lose essential medical aids such as insulin pens and many do not bring prescriptions with them when evacuated.. Since medication loss is partly a responsibility of evacuees, understanding the impact of medication loss may lead to raising awareness and better preparations among the patients and health care professionals. People who are not prepared could have worse outcomes and many risk dying when their medication is not available.
Funding Statement
This project was not funded. The authors have declared that no competing interests exist.Introduction
After an extreme weather event or other natural hazard, the continuity of routine care is one of many challenging aspects of post disaster healthcare. Although a disaster can impact on all available services, healthcare facilities can be overwhelmed reducing their ability to maintain normal function. Structural and non-structural damage to their buildings, creating an insecure environment for hospital staff, and disruption of supply chains, all lead to closure of wards for new admissions, or even evacuation of patients and staff, at a time when they are critical for those who are injured by the disaster. Recognising the impact of extreme events on healthcare facilities, normal functioning is still required for people needing routine health management such as oncological treatment, dialysis and maternity care, as well as those people with chronic conditions who require daily medication to maintain their wellbeing.
Long-term non-communicable diseases 1 are increasing with a growing and ageing world population and in 30 years from 1990, NCD’s are estimated to increased 1.8 times 2. Ensuring continuation of routine care for chronic conditions will be an increasing burden during and post disaster periods both in developing and developed countries 3. Interruption of routine medication lead can lead to an exacerbation of chronic conditions such as insulin-dependent diabetes 4 and infectious diseases for example tuberculosis 5. This can also potentially cause secondary life-threatening outcomes as a result of the deterioration of chronic conditions such as ischemic heart diseases among patients with hypertension 6, and low compliance to medication regimens in the future 7,8.
During any disaster, medication maintenance is problematic due to people not having adequate dosages for a sufficient period of time, not having prescriptions with them, not remembering the medication they are on and more likely not having any medication with them at all. These people have been described as ‘drug refugees’. In the Great East Japan Earthquake in 2011, for example, a large number of ‘drug refugees’ were reported 9, and at least 283 people were reported to have died from the exacerbation of pre-existing conditions due to lack of access to healthcare 10. The health impacts on drug refugees has had, little research conducted among the affected population.
Since medication loss is partly a responsibility of evacuees, understanding the impact of medication loss may lead to raising awareness and better preparations among the patients and health care professionals. The aim of this systematic literature review was to identify the extent and implications of medication loss and the burden of prescription refill on medical relief teams following extreme weather events and other natural hazards.
Methods
The search strategy followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement where applicable, and this checklist was used in designing and reporting our review 11.
Identification
The key health journal databases (Medline, Embase, PsycINFO, Maternity and Infant Care, and Health Management Information Consortium (HMIC)) were searched via the OvidSP search engine. Search terms were identified by consulting MeSH terms. The validity of the search was confirmed by comparing the generated results to articles obtained from expert consultation and ‘snow-ball’ search). After this pilot search, it was revealed that using only MeSH terms was not sufficient to identify all relevant articles. Therefore, key words related to disaster and medication were added to MeSH term search as shown in Table 1. The relevant articles were searched by combining [Terms for disasters] AND [Terms for medications].
Search Area
Term Category
Terms
MeSH terms
Disaster
Disasters
Disaster medicine
Disaster planning
Emergencies
Emergency shelter
Relief work
Medication
Chronic disease
Community-based participatory research
“Delivery of health care”
Drug prescriptions
Drug utilization
“Health services needs and demand”
Health services accessibility
Medication adherence
Needs assessment
“Patient acceptance of health care”
Patient compliance
Pharmaceutical preparations
Prescriptions
Prescription drugs
Key words
Disaster
Disaster$
Earthquake/Earthquakes
Evacu$
Flood/Floods
Hurricane/Hurricanes
Landslide/Landslides
Tsunami
Typhoon/Typhoons
Volcan$
Wildfire/Wildfires
Medication
Prescri$
Chronic disease/diseases
Chronic condition/conditions
Medication/medications
Needs assessment/assessments
Limitations specified when searching the literature: Human; Date of publication from 2003-2013; English Language; with abstract
Eligibility criteria
1) Inclusion criteria
Articles were eligible if they were published over the period from January 2003 to August 2013, were written in English, and included an abstract. We limited the search period to10 years because technology and needs for chronic diseases such as dialysis and home oxygen therapy treatments have changed over this period of time. Eligible articles described the following: (i) evacuees’ actions of bringing prescription medications with them; (ii) burden of prescription refills or prescription of medication for chronic conditions within relief activities after disasters, and/or (iii) disruption of medications due to evacuees not bringing their medications.
2) Exclusion criteria
Articles and papers were excluded if they were (i) abstracts for conferences or dissertations; (ii) chapters of books; and (iii) articles written in a language other than English.
Study selection
The search was conducted on 5th September, 2013 and generated 5,382 results of which 1,652 were duplicates and removed, leaving 3,730 records, Out of these records 2,961 were apparently irrelevant when screened by title exclusion criteria. Hence, the initial screening by title identified 811 records as relevant and for these remaining articles, abstracts were checked independently by SO and other co-authors (SH and LM). Abstract eligibility screening excluded a further 513, however, given the wide range of sources searched, an additional 66 abstracts were added as a result of citation searching, shown as ‘secondary screening’ in Figure 1. Overall, a total of 364 articles were identified. The full-text articles eligibility screening identified those not fulfilling the inclusion criteria which totalled 294, thus leaving a total of 70 articles for this systematic review (Figure 1).
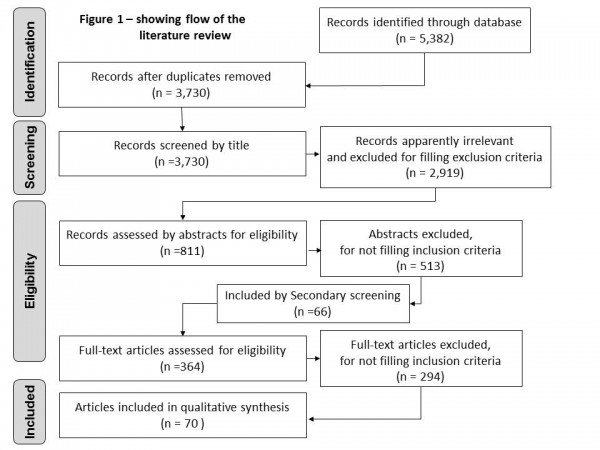
Fig. 1: Study selection flow chart
Risk of bias and data synthesis
Most of the data collected were from observational studies using convenience population samples because obtaining robust data from appropriate population samples is almost impossible immediately after an extreme event. Due to the heterogeneity of the data, no formal assessment of bias in each study was made. In addition, due to the wide variety of the targeted populations, statistical data synthesis was considered inappropriate.
Results
This is the first systematic review that has addressed the topic of medication needs in disaster driven evacuation. Most of these publications did not focus on the medications needs from disaster driven evacuation thus the information was limited and often not covered comprehensively. Although the results are provided in detail below the findings are used principally to inform a detailed commentary of the assimilated results from the many publications identified.
From the MeSH terms, 70 papers were identified of which 69 articles were related to extreme events. These events showed a wide range of disasters occurring from 1992 to 2011 and included 14 hurricanes, typhoons or cyclones; eight earthquakes; two flooding; one wildfire; and one power outage and one conflict (Table 2). There were 29 (44%) articles that reported on the impacts from the 2005 Hurricane Katrina. Additionally 54 (78%) of the disasters identified occurred in the United States of America (USA), a total of nine countries were found to have reported these extreme events.
Year
Month
Name of events
Country
No. of articles
1992
August
Hurricane Andrew
US
4
1992
September
Hurricane Iniki
US
3
1994
January
Northridge earthquake
US
1
1995
January
Hanshin earthquake
Japan
1
1998-1999
–
Kosovo crisis
Kosovo
2
2001
January/February
El Salvador earthquakes
El Salvador
1
2001
June
Tropical Storm Allison
US
3
2003
August
New York Blackout
US
1
2003
December
Bam earthquake
Turkey
1
2004
April
Typhoon Sudal
Micronesia
1
2004
August
Hurricane Charley
US
1
2004
August-September
Hurricane Frances
US
1
2004
September
Hurricane Ivan
US
1
2004
September
Hurricane Jeanne
US
1
2004
October
Mid-Niigata Prefecture earthquake
Japan
1
2005
August
Hurricane Katrina
US
29
2005
September
Hurricane Rita
US
2
2005
October
Pakistan earthquake
Pakistan
1
2005
October
Hurricane Wilma
US
2
2006
October
Flash flood in Japan
Japan
1
2007
October-November
California Wildfire
US
1
2008
June
Flooding in Iowa
US
1
2008
August-September
Hurricane Gustav
US
1
2008
September
Hurricane Ike
US
1
2010
January
Haiti earthquake
Haiti
1
2011
February
Cyclone Yasi
Australia
1
2011
March
Great East Japan Earthquake
Japan
3
–
–
Not specific
2
Total
27 events
9 countries
69 articles
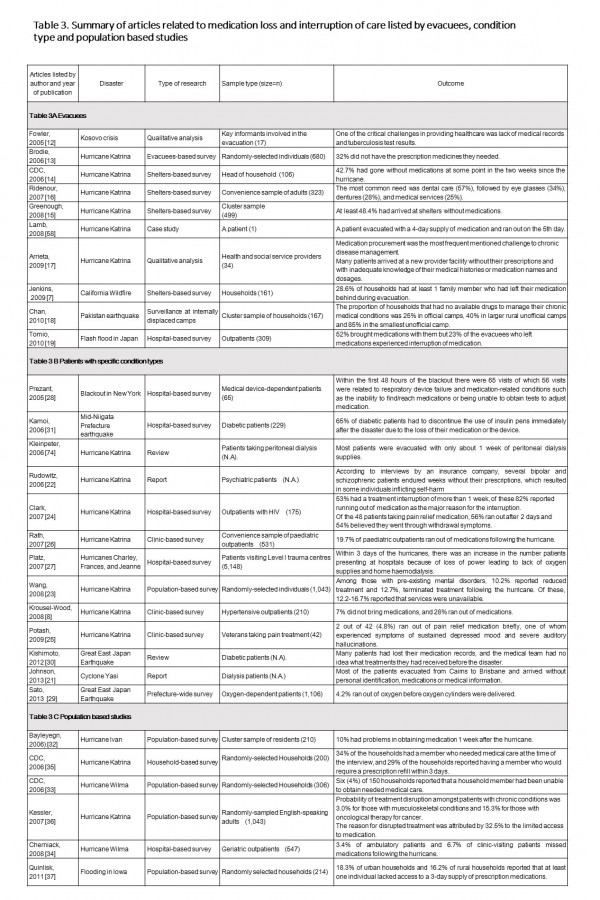
Table 3 is a summary of articles related to medication loss and interruption of care listed by evacuees, condition type and population based studies and lists chronologically the type of disaster, study method, sample and sample size for this systematic review where relevant. There are three sections within Table 3 and within each section there is an account of the outcome of each report relating to medication loss, medication unavailability and not having an adequate supply.
Table 3
Table 3A Evacuees
A significant proportion of evacuees from, or residents at, disaster areas lost their medication.
In the first study chronologically, Fowler et al.,12 reported from interviews with humanitarian workers involved in the evacuation after the Kosovo crisis in 1999, which revealed that one of the critical challenges in providing healthcare was the lack of medical records and tuberculosis (TB) test results. From the six studies involving Hurricane Katrina it is possible to determine that a major proportion of people did not have adequate medication supplies, an issue identified in five of these papers. In three studies the percentage of those without medication were identified, namely 32% by Brodie et al. 13; 42.7% by CDC 14 and 48.4% by Greenough et al. 15. In addition the questionnaire-based survey amongst evacuees who arrived at a family assistance centre two weeks after Hurricane Katrina revealed that the 42.7% had run out of their medications even when they brought them 14. In another study Ridenour et al., 16 reported that, from a convenience sample of 323 adults, 57% of people required dental care, 34% eye glasses, 28% denture and 25% medical services. In the final paper in this category from Hurricane Katrina, Arrieta et al. 17 reported that medication procurement was the most frequent mentioned challenge to chronic disease management and that ‘ many patients arrived at a new provider facility without their prescriptions and with inadequate knowledge of their medical histories or medication names and dosages’.
The remaining publications in this section related to a Californian wildfire, the Bam earthquake and flash floods in Japan. Data from California showed that patients did not have their medications with them during evacuation for one family member in 28.6% of households 7. Information from a cluster sample of households following the Bam earthquake reported that 25% of people in in official camps, 40% in larger rural unofficial camps and 85% in the smallest unofficial camp had no available drugs to manage their chronic medical conditions 18. After the flash floods in Japan in 2006, 48% of the evacuees left their medication and 88% left their prescription records behind 19.
Table 3B Patients with specific condition types
In this section, the focus was on people with specific medical conditions and availability of continued medication treatment following an extreme event. Eight articles focussed on hurricanes in the USA, seven were related to Hurricane Katrina and one article covered the impact of three consecutive hurricanes in Florida. Other articles in this section covered a power outage in New York, earthquakes in Japan and a cyclone in Queensland, Australia.
Following Hurricane Katrina evacuees on peritoneal dialysis were asked to bring with them approximately 1 week supply of personal medical supplies 20; however, some dialysis patients evacuated from Cairns to Brisbane during cyclone Yasi arrived without personal identification, medications or medical information 21.
Mental health impact reports following Hurricane Katrina showed that some psychiatric patients inflicted self-harm as a result of not having prescriptions filled 22. A telephone interview with randomly-selected English-speaking adult Katrina survivors in New Orleans, Alabama, Louisiana, and Mississippi indicated that 21.3% had a pre-existing mental disorder, of whom 10.2% had reduced, and 12.7% terminated, their treatment because of the hurricane 23.
Again from Hurricane Katrina reports, treatment interruption occurred for more than 1 week for 53% of people with HIV, of which 82% reported the interruption being due to their medication running out, further, 48 patients from this study who were taking pain relief medication 56% ran out after 2 days and 54% believed they were going through withdrawal symptoms 24. In another study, Potash et al. 25 reported that 4.8% of people ran out of their pain relief medication which caused one person to experience severe side effects from not having this medication. Rath et al. 26 reported that 19.7% of paediatric outpatients ran out of medications, while 7% of patients with hypertension did not bring their medication with them and 28% ran out of their supply 8.
In Florida following the three Hurricanes of Charley, Frances and Jeanne there was an increase in the number patients presenting at hospitals because of loss of power leading to lack of oxygen supplies and home haemodialysis 27.
During the New York blackout, within 48 hours the Emergency Department of Montefiore Medical Center reported that 56 out of 65 visits were related to respiratory device failure and that medication-related problems were due to people unable to find or reach medications or were unable to obtain tests needed to adjust medications such as warfarin 28.
In Japan during the following the Great East Earthquake 4.2% of people ran out of oxygen before a new supply of oxygen cylinders could be delivered 29. Kishimoto and Noda 30 noted that many diabetic patients had lost their medication records, and the medical team could not determine what treatments they had received before the disaster. After the Mid-Niigata earthquake in Japan in 2004, hospital-based survey reported that 65% of patients with type 1 diabetes with insulin therapy were unable to continue the use of insulin pens due to medication loss immediately after the earthquake 31.
Table 3C Population based studies
In this section six reports focus on groups of people and their medication treatment in the USA following Hurricanes Ivan, Katrina and Wilma and the flooding in state of Iowa.
Bayleyegn et al. 32 reported that 10% of a cluster sample of 210 people had problems obtaining medication 1 week following Hurricane Ivan. After Hurricane Wilma, six (4%) of 150 households surveyed, reported that a household member had been unable to obtain needed medical care 33 and Cherniack et al. 34 reported that 10.1% of patients missed medications after the hurricane. Following Hurricane Katrina surveys showed that 34% of the households had a member who needed medical care at the time of the interview, and who would require a prescription refill within 3 days 35. Kessler et al. 36 noted that treatment was disrupted for patients with musculoskeletal conditions (3.0%) and those with oncological conditions (15.3%) and that 32.5% attributed this disruption to the limited access to medication.
Following the floods in Iowa, 18.3% of urban households and 16.2% of rural households reported that at least one individual lacked access to a 3-day supply of prescription medications 37.
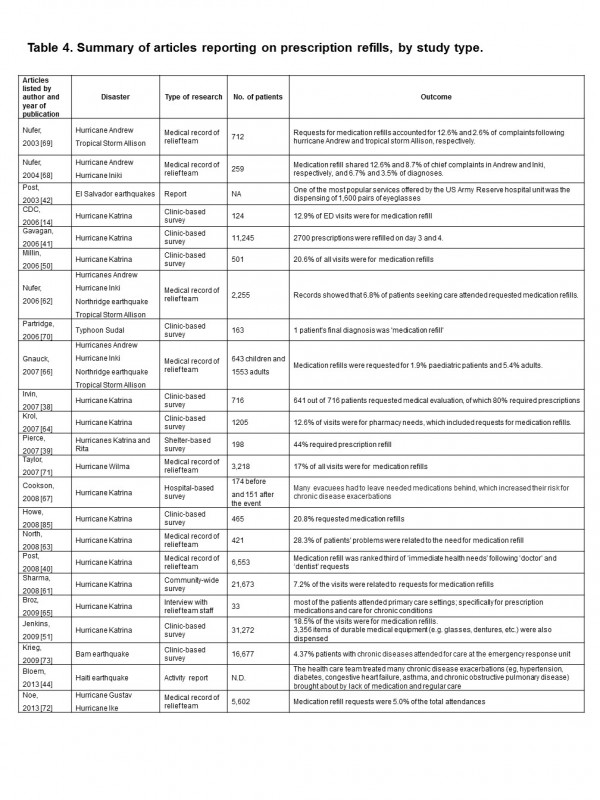
Table 4
Table 4 is a summary of articles reporting on prescription refills, by study type and lists chronologically the disaster, type of research, number of patients and the relevant outcome from each study.
Twenty-three articles described patients coming to field clinics or emergency hospitals for prescription refills. In each article listed, where available, the frequency of refill request percentage by study is documented. Details of some of the studies and their most relevant findings are summarised briefly below:
Table 5
Routine medications
E.g. prescription medications for hypertension, diabetes, etc. See Table 4 for references.
Medical records
List of medications (Clark et al., 2007; Kamoi et al., 2006; Kishimoto and Noda, 2012; Krousel-Wood, 2009; Lach et al., 2005)
Medication logs (e.g. chemotherapy) (Imamura and Ueno, 2011)
Laboratory data (e.g. Tuberculosis test results, CD4+ T-cell counts for HIV patients) (Fowler et al., 2005)
Allergy information (Fung and Loke, 2010)
Style and serial numbers of the devices (e.g. pacemakers) (Lach et al., 2005)
Devices for specific care
Devices for insulin delivery (e.g. needles, glucose-sensor, cartridge),(Jenkins et al., 2009b; Kamoi et al., 2006; Miller and Arquilla, 2008)
Nebulizer machines (Jenkins et al., 2009b)
CPAP machines (Jenkins et al., 2009b)
Power generator / automobile with inverter for electrical device (Tanaka, 2013)
Oxygen cylinders/concentrators (Jenkins et al., 2009b)
Canned nutritional supplements for the tube feedings (Mace et al., 2010)
Devices for daily life
Glasses (Lach et al., 2005; Sakashita et al., 2013)
Hearing aids (Lach et al., 2005)
Canes (Jenkins et al., 2009b)
Walkers (Jenkins et al., 2009b)
Wheel chairs (Lach et al., 2005)
Dentures (Lach et al., 2005; Sareen and Shoaf, 2000)
Emergency medications
e.g. potassium-binding resin for patients taking dialysis (Foster et al., 2011; Millin et al., 2006)
Over-the-counter (OTC) medications
Painkillers/medication for fever (Fung and Loke, 2010)
Anti-histamine agents (Fung and Loke, 2010)
Others
Personal identifier for those who cannot speak (Andersson et al., 2006)
Medication opening devices for those with hand disabilities (Mori et al., 2007)
The most challenging part to bringing medication is ensuring a patient carries the full range of medication they need, including medical records, emergency drugs and life-support devices. Examples of the range of medications required following a disaster and evacuation was drawn from the reviewed articles, and is summarised in Table 5.
Medical records are critical in some situations, such as CD4 cell count and HIV RNA levels for HIV patients 24 medication logs for cancer patients 45 and Tb test results 12. Even for other patients, medical records including allergy to medications 24,30,31,46,47 are essential. For patients with specific medical devices such as pacemakers, style and serial numbers of the devices is important 47. It is recommended that individuals keep a list of these essential items , which should be reviewed updated periodically 46 and the list preferably kept it in wallet or purse, which is likely to be brought along during an emergency 48.
Prescriptions specific to emergency situations should also be considered for each patient. For example, dialysis patients need to bring a potassium-exchanging resin, which is essential to reduce the potassium level when the access to dialysis is limited 49,50. Devices for insulin injection (vials, needles or pens with replaceable cartridges of insulin) 31, gluco-metres 4,31,51, fluids and devices for peritoneal dialysis, 20 nebuliser machines, CPAP machines, oxygen cylinders, 51 batteries for aspirators and artificial ventilators 52, suctioning and tube feedings, and canned nutritional supplements for the tube feedings 53 should also be considered as part of the emergency pack for patients to bring. For the families with children who are dependent on technology and electrical devices, it seems more difficult to prepare for all the life-supporting equipment required, such as power generator or car/vans that can be used to generate electricity 54.
Supportive tools for daily life, such as wheel chairs, hearing aids 47, canes, walkers, 51 dentures, glasses 43,47, extra batteries for wheelchairs and other assistive devices, and incontinence briefs for the elderly 47 are often lost at the time of evacuation. For those who cannot speak, bringing a personal identifier is also critical 55. Over-the-counter medicines, such as medication for fever or pain, anti-histamine for allergy, denture adhesive, and sanitary products are also important when access to pharmacies are disrupted 56. For those with hand disabilities, openers for the medications are also an essential item 57.
Discussion
This systematic review revealed that a considerable number of patients lose their medication during evacuation. As a result, medication refill is an immediate health need, making the prescription of medications for pre-existing conditions an increasing burden of medical relief activities at a time when acute needs are also over-whelming. At the current time, preparedness with respect to medications for disasters is not fully appreciated nor given much attention by those requiring daily and constant medication; meaning that a large number of patients facing extreme events could have avoided prescription interruption had they not lost their medication and or medical devices. Until individuals, with the assistance of their healthcare providers, undertake preparative actions, those organising relief activities need to be prepared to cope with emerging treatment alongside the management of chronic illnesses, including medication refills and devices.
The discussion is presented by a) the impact of medication loss and interruption of care, b) the impact of prescription refill post disaster and c) the value of effective preparation actions.
a) The impact of medication loss and interruption of care
Studies from developed countries show that the impact of medication loss and interruption of care can be a significant issue. From the results above, it is possible to demonstrate that surveys targeting paediatric patients in New Orleans after Hurricane Katrina revealed that 33.9% of evacuated children with pre-existing chronic conditions ran out of medication; 26 as a result, 58.4% experienced at least one disruption to care. In a questionnaire-based survey of geriatric patients visiting a hospital in Florida one year after Hurricane Wilma, 3.4%-6.7% reported that they had missed medication within two weeks of the event 34. Some studies found that although some people brought their medication with them upon evacuation, they had only brought enough supply for a limited period 58. After Hurricane Ivan in 2004, 10% of households in most affected counties had problem obtaining medication one week after the storm, thus bringing sufficient supply may have be difficult 32. After the Great East Japan Earthquake and the following tsunamis in 2011, many evacuees had no time to gather their belongings. Some of them were treated with unique medication, such as immuno-suppressants, which were not obtainable at the disaster area. As a result, these patients had to stop their medication for weeks knowing that their medical conditions would deteriorate 59.
The problem regarding medication loss is not limited to developed countries. Among the internally-displaced population from the 2005 Pakistan earthquake, 85% of the households in small unofficial camps had no available drugs to manage their chronic medical conditions. After the Haiti earthquake in 2010, a relief team reported treating many women for chronic disease exacerbations brought about by lack of medication and/or regular care 44.
Some articles reported medication by specific chronic condition, which showed that the level of preparation may vary by conditions. People with mental illness are also at high risk of medication interruption 23,1.
Examples of loss of medication lists and medical devices were identified as medical and life-support devices are as important as technological tools like haemodialysis and oxygen. A questionnaire conducted on the evacuees two weeks after Hurricane Katrina revealed that medical services were only the fourth most commonly reported medical need. The most common was dental care (57% of the respondents), followed by eyeglasses (34%) and dentures (28%). Other devices needed were hearing aids, canes, wheel-chairs, and walkers 16.
b) The impact of prescription refill post-disaster
The high prevalence of the need of prescriptions becomes a burden on medical teams at the disaster area which was identified in Table 4. For example, an analysis of survey data after Hurricane Katrina revealed 7.2% of the patients visiting emergency treatment facilities within 2 months of the hurricane were attending for medication refill 61.
Looking at the timeline of health needs following a disaster, the proportion of medication refills does not appear to change between the early and late stage of the relief activities. For example, according to a retrospective review on the patients seen by a Disaster Medical Assistance Team during four extreme events in New Mexico, US, the proportion of the patients visiting for medication refill was 6.0% within 7 days from the events and 7.6% after 7 days 62. Even for specialty care, medication refill often shares a significant part of relief activities. After Katrina, of 421 patients who were seen by mental health professionals, 119 (28.3%) were attending for medication refill 63.
Despite medication refills being a common need among the disasters studied, the proportions of patients coming to health facilities for medication refill vary within and between events. For example 20.9% in a Louisiana clinic site two weeks after the event, 50, within 2 months 20.8% in a temporary clinic in New Orleans 24, 12.6% in the mobile medical units within 3 weeks, 64 and 48% in medical units in Chicago between 1-4 weeks after the event. 65
Additionally, a comparison between disasters suggested the burden differs depending on the scale and types of the disasters 66 For example, Cookson et al. 67 reported that non-significant increases were seen with medication refill request after the Katrina. In other cases, the proportion requiring medication refill was reported to be 3.5-3.6% after the Hurricane Iniki in 1992 66,68, 6.7%-10.0% after the Hurricane Andrew in 1992 66,68, 1.3-3.7% after Tropical Storm Allison in 2001, 66,69 0.6% after Typhoon Sudal in Micronesia in 2004 70, 7% after the Hurricane Wilma in 2005, 71 and 4.8-7.1% after Hurricanes Gustav and Ike in 2008 72. Another example from the Bam Earthquake in Iran in 2003 showed that the management of ‘chronic disease under treatment’ when measured required only 4.37% of the tasks of the emergency response unit. 73.
c) The value of effective preparation actions
Although the main scope of the review was to identify patients’ reactions relating to bringing their medications during a disaster, several implications for effective preparedness were identified.
Twelve articles described possible effective preparation actions for patients. Having a personal stockpile is recommended in many articles, though the recommended personal stockpile ranges from 3-4 days 20,74 to 1 month 75. In a survey study conducted in California, US, the proportion of those who had a 2-week supply of medication ranged from 60.1% among non-veteran women to 81.9% among veteran men 76. It was customary in India for pregnant women (81.1% reported) to have individual stockpile of their routine medications 77.
However, just keeping extra doses of medication stockpiled is likely to have limited impact. In a hospital-based survey study targeting evacuated outpatients from the Japanese flash flood in 2005, keeping a personal stockpile did not increase the likelihood of bringing medications to the evacuated sites 19. On the other hand, those who had prepared an emergency pack were 5.7 times more likely to bring medications to the evacuated sites 19. Therefore, the researchers recommended that the stockpile is packed in a bag for easy access. Even so, the compliance for making an emergency pack seems to be low. For example, 63% of the haemodialysis patients in California had a 2-week supply of medicines but only 31% stored the items in an emergency pack. 49 In a study targeting patients with rheumatoid arthritis in Japan, 46% reported they had a personal stockpile of their medications but only 25% had packed an emergency bag 78. Other researchers reported that although 82.8% of households with children had stocked common medication for fever or pain for 3days, only 60.6% kept a first aid box and only 14.6% thought they would take their medications during evacuation 56.
Carrying medications at all time 58,78,79 or keeping extra medication in multiple places, such as schools and offices 80, are described as the most robust and effective emergency plan for patients. However, low compliance with this action has been reported. Among the rheumatoid arthritis patients in Japan, only 53% of those who had a personal stockpile carried their medication all the time 78. Among HIV patients, 33% of patients did not have individual health cards at the time of interview, potentially making the provision of therapy to these patients difficult 19,79.
Although having a personal stockpile is recommended by the Centres for Disease Control and Prevention (CDC) and the American Red Cross 81, our review implies that just having a personal stockpile might not be effective 78. Many onsite workers recommend patients should have an emergency bag. For example, a station manager at The Hampshire Fire & Rescue Service in the United Kingdom (UK) remembered: ‘after fires, many people had to go back to their home to get medications and medical devices they need.’ He said that if communities can be educated in advance they will be able to prepare an emergency ‘grab bag’ containing vital personal items such as prescription medicines and medical devices and glasses/contact lenses, and suggests that this increases the likelihood of bring medicines/devices during a disaster 82.
To achieve patients’ preparedness, healthcare professionals play an essential role in establishing effective emergency planning for patients.
Other stakeholders, such as policy makers and researchers, should also coordinate around patients’ emergency planning (Figure 2). Recently, an increasing effort has been made by national and local governments in several countries to encourage patients to prepare an emergency bag. For example, in the UK, the National Health Service provides discharged patients with a carry bag (‘green bag’) for their medications to encourage patients to bring their medication in emergency situations 82, which is applicable to the time of evacuation. In the US, the CDC and American Red Cross raised ‘gather emergency supplies’ as the first step for emergency preparedness 85,86.
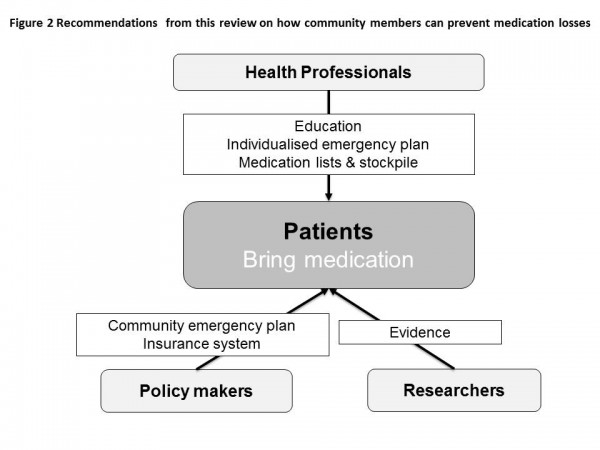
Fig. 2: Recommendations on how community members can prevent medication losses
Even so, evidence is still weak with regard to preparedness actions by patients and the efficacy of intervention to encourage preparation. Researchers should be actively involved in disaster plans to leverage the preparedness among patients. For example, health impacts caused by loss of medication should be assessed using feasible and standardised methods to enable targeted aid following a disaster. Baseline data should also be measured and made available to appropriate agencies, including the burden of chronic diseases in each community 87,88, health care disparities 89, vulnerable populations for whom preparedness is a challenge 90, preparedness of general or specific groups of people 34,37 as well as factors that affect emergency preparedness 91. Intensive research following disasters is also critical, and should include rapid health needs assessment among the evacuees, 37,61 health impact assessment including medication adherence 92, and evaluation of the efficacy of preparedness actions 90 to inform future planning and preparation.
The key findings and recommendations are summarised in Box 1.
Box 1. Summary of key findings DRR – disaster risk reduction; DRM – disaster risk management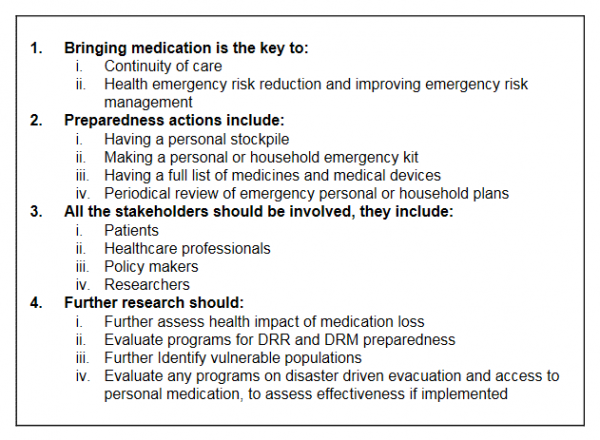
Limitations
The most significant limitation of this study is lack of comparative data. There is no standardised way of measuring the impact of bringing medication at evacuation. Most frequently, survey is conducted on convenience samples, which makes it hard to generalise beyond that particular population. After a disaster, obtaining quality data is challenging due to the flow of evacuees and temporary nature of their status, lack of personnel, and ethical concerns accompanying the conduct of research on suffering people. Simple, unobtrusive and feasible approaches of monitoring preparedness and health outcomes should be carefully designed and established before disasters occur, especially in those regions subject to frequent disasters.
Another limitation is publication bias; most of the relevant articles were from the US, and a large proportion specifically focused on hurricane Katrina. Whether the issue of medication loss is less a problem in developing countries or simply less frequently studied and/or published is not clear. There is a clear need for evidence from all over the world, and from the most marginalised, thus rarely reported, populations.
This research does not focus on longer term crises, such as drought or political and economic failures, in which restoration of healthcare provision may take many months 5. In such disasters, other issues may predominate, and preparing and bringing a stockpile of medication/medical devices may not be the best solution.
Conclusion
To achieve patients’ preparedness, healthcare professionals play an essential role in establishing effective emergency planning for patients should provide patients with medications and other resources sufficient for disaster preparedness as well as up-to-date medical records. Health professionals have a responsibility to educate patients about the potential health impacts of medication interruption, emphasising that bringing medication and medical records may be the only way to enable them to continue normal care in an emergency. They must help patients to design an individualised and practical emergency plan that takes in to account patient-specific barriers such as forgetfulness. In disasters for which there is some advance warning, such as hurricanes, health professionals may make contact with patients reminding them to bring their medication and medical records when they evacuate. Front-line public health workers and the members of rescue teams should have adequate medication for their own medical conditions to sustain them for the duration of their rescue efforts during a disaster.
People may survive the initial disaster but if they are not educated or appropriately prepared in particular when medication is involved they may not survive the aftermath.
Appendix 1
PRISMA Checklist
References
- WHO (2011) Global status report on noncommunicable diseases 2010. Geneva, Switzerland: World Health Organization.
Reference Link - Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997 May 24;349(9064):1498-504. PubMed PMID:9167458.
- Chan EY, Kim J. Chronic health needs immediately after natural disasters in middle-income countries: the case of the 2008 Sichuan, China earthquake. Eur J Emerg Med. 2011 Apr;18(2):111-4. PubMed PMID:20679898.
- Miller AC, Arquilla B. Chronic diseases and natural hazards: impact of disasters on diabetic, renal, and cardiac patients. Prehosp Disaster Med. 2008 Mar-Apr;23(2):185-94. PubMed PMID:18557300.
- Veenstra N, Whiteside A, Lalloo D, Gibbs A. Unplanned antiretroviral treatment interruptions in southern Africa: how should we be managing these? Global Health. 2010 Mar 31;6:4. PubMed PMID:20356383.
- Murakami H, Akashi H, Noda S, Mizoue T, Okazaki O, Ouchi Y, Okaji Y, Kajiwara C, Miyoshi C. A cross-sectional survey of blood pressure of a coastal city's resident victims of the 2011 Tohoku tsunami. Am J Hypertens. 2013 Jun;26(6):799-807. PubMed PMID:23455946.
- Jenkins JL, Hsu EB, Sauer LM, Hsieh YH, Kirsch TD. Prevalence of Unmet Health Care needs and description of health care-seeking behavior among displaced people after the 2007 California wildfires. Disaster Med Public Health Prep. 2009 Jun;3(2 Suppl):S24-8. PubMed PMID:19491584.
- Krousel-Wood MA, Islam T, Muntner P, Stanley E, Phillips A, Webber LS, Frohlich ED, Re RN. Medication adherence in older clinic patients with hypertension after Hurricane Katrina: implications for clinical practice and disaster management. Am J Med Sci. 2008 Aug;336(2):99-104. PubMed PMID:18703901.
- Ochi S, Murray V, Hodgson S. The great East Japan earthquake disaster: a compilation of published literature on health needs and relief activities, march 2011-september 2012. PLoS Curr. 2013 May 13;5. PubMed PMID:23787732.
- Cabinet Office GoJ (2012) Report on the Great East Japan earthquake related to mortality (title translated 東日本大震災等に係る状況). 18th Subpanels on medical affairs, Social Security Council. Tokyo: Cabinet Office, Government of Japan.
Reference Link - Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009 Aug 18;151(4):264-9, W64. PubMed PMID:19622511.
- Fowler N, Redwood-Campbell L, Molinaro E, Howard M, Kaczorowski J, Jafarpour M, Robinson S. The 1999 international emergency humanitarian evacuation of the Kosovars to Canada: A qualitative study of service providers' perspectives at the international, national and local levels. Int J Equity Health. 2005 Jan 12;4(1):1. PubMed PMID:15647108.
- Brodie M, Weltzien E, Altman D, Blendon RJ, Benson JM. Experiences of hurricane Katrina evacuees in Houston shelters: implications for future planning. Am J Public Health. 2006 Aug;96(8):1402-8. PubMed PMID:16571686.
- Illness surveillance and rapid needs assessment among Hurricane Katrina evacuees--Colorado, September 1-23, 2005. MMWR Morb Mortal Wkly Rep. 2006 Mar 10;55(9):244-7. PubMed PMID:16528233.
- Greenough PG, Lappi MD, Hsu EB, Fink S, Hsieh YH, Vu A, Heaton C, Kirsch TD. Burden of disease and health status among Hurricane Katrina-displaced persons in shelters: a population-based cluster sample. Ann Emerg Med. 2008 Apr;51(4):426-32. PubMed PMID:17583378.
- Ridenour ML, Cummings KJ, Sinclair JR, Bixler D. Displacement of the underserved: medical needs of Hurricane Katrina evacuees in West Virginia. J Health Care Poor Underserved. 2007 May;18(2):369-81. PubMed PMID:17483565.
- Arrieta MI, Foreman RD, Crook ED, Icenogle ML. Providing continuity of care for chronic diseases in the aftermath of Katrina: from field experience to policy recommendations. Disaster Med Public Health Prep. 2009 Oct;3(3):174-82. PubMed PMID:19865042.
- Chan EY, Kim JJ (2010) Characteristics and health outcomes of internally displaced population in unofficial rural self-settled camps after the 2005 Kashmir, Pakistan earthquake. Eur J Emerg Med 17: 136-141.
- Tomio J, Sato H, Mizumura H (2010) Interruption of medication among outpatients with chronic conditions after a flood. Prehosp Disaster Med 25: 42-50.
- Kleinpeter MA, Norman LD, Krane NK (2006) Disaster planning for peritoneal dialysis programs. Advances in peritoneal dialysis Conference on Peritoneal Dialysis 22: 124-129.
- Johnson DW, Hayes B, Gray NA, Hawley C, Hole J, et al. (2013) Renal services disaster planning: Lessons learnt from the 2011 Queensland floods and North Queensland cyclone experiences.
- Rudowitz R, Rowland D, Shartzer A (2006) Health care in New Orleans before and after Hurricane Katrina. Health Aff (Millwood) 25: w393-406.
- Wang PS, Gruber MJ, Powers RE, Schoenbaum M, Speier AH, et al. (2008) Disruption of existing mental health treatments and failure to initiate new treatment after Hurricane Katrina. The American Journal of Psychiatry 165: 34-41.
- Clark RA, Mirabelli R, Shafe J, Broyles S, Besch L, et al. (2007) The New Orleans HIV outpatient program patient experience with Hurricane Katrina. The Journal of the Louisiana State Medical Society : official organ of the Louisiana State Medical Society 159: 276, 278-279, 281.
- Potash MN, West JA, Corrigan S, Keyes MD (2009) Pain management after Hurricane Katrina: outcomes of veterans enrolled in a New Orleans VA pain management program. Pain Med 10: 440-446.
- Rath B, Donato J, Duggan A, Perrin K, Bronfin DR, et al. (2007) Adverse health outcomes after Hurricane Katrina among children and adolescents with chronic conditions. Journal of health care for the poor and underserved 18: 405-417.
- Platz E, Cooper HP, Silvestri S, Siebert CF (2007) The impact of a series of hurricanes on the visits to two central Florida Emergency Departments. Journal of Emergency Medicine 33: 39-46.
- Prezant DJ, Clair J, Belyaev S, Alleyne D, Banauch GI, et al. (2005) Effects of the August 2003 blackout on the New York City healthcare delivery system: a lesson for disaster preparedness. Crit Care Med 33: S96-101.
- Sato K, Morita R, Tsukamoto K, Sato N, Sasaki Y, et al. (2013) Questionnaire survey on the continuity of home oxygen therapy after a disaster with power outages. Respir Investig 51: 9-16.
- Kishimoto M, Noda M (2012) The Great East Japan Earthquake: Experiences and Suggestions for Survivors with Diabetes (perspective). PLoS Curr 4: e4facf9d99b997.
- Kamoi K, Tanaka M, Ikarashi T, Miyakoshi M (2006) Effect of the 2004 Mid Niigata Prefecture earthquake on glycemic control in type 1 diabetic patients. Diabetes research and clinical practice 74: 141-147.
- Bayleyegn T, Wolkin A, Oberst K, Young S, Sanchez C, et al. (2006) Rapid assessment of the needs and health status in Santa Rosa and Escambia Counties, Florida, after Hurricane Ivan, September 2004. Disaster Management and Response 4: 12-18.
- Rapid needs assessment of two rural communities after Hurricane Wilma--Hendry County, Florida, November 1-2, 2005. MMWR Morb Mortal Wkly Rep. 2006 Apr 21;55(15):429-31. PubMed PMID:16628183.
- Cherniack EP, Sandals L, Brooks L, Mintzer MJ (2008) Trial of a survey instrument to establish the hurricane preparedness of and medical impact on a vulnerable, older population. Prehosp Disaster Med 23: 242-249.
- Rapid community needs assessment after Hurricane Katrina--Hancock County, Mississippi, September 14-15, 2005. MMWR Morb Mortal Wkly Rep. 2006 Mar 10;55(9):234-6. PubMed PMID:16528229.
- Kessler RC, Wang PS, Kendrick D, Lurie N, Springgate B (2007) Hurricane Katrina's impact on the care of survivors with chronic medical conditions. Journal of General Internal Medicine 22: 1225-1230.
- Quinlisk P, Jones MJ, Bostick NA, Walsh LE, Curtiss R, et al. (2011) Results of rapid needs assessments in rural and urban Iowa following large-scale flooding events in 2008. Disaster Med Public Health Prep 5: 287-292.
- Irvin CB, Atas JG (2007) Management of evacuee surge from a disaster area: solutions to avoid non-emergent, emergency department visits. Prehosp Disaster Med 22: 220-223.
- Pierce JR, Jr., Pittard AE, West TA, Richardson JM (2007) Medical response to hurricanes Katrina and Rita: local public health preparedness in action. J Public Health Manag Pract 13: 441-446.
- Post DE, Kasofsky JM, Hunte CN, Diaz JH (2008) A regional human services authority's rapid needs assessment of evacuees following natural disasters. American journal of disaster medicine 3: 253-264.
- Gavagan TF, Smart K, Palacio H, Dyer C, Greenberg S, et al. (2006) Hurricane Katrina: Medical response at the Houston astrodome/reliant center complex. Southern medical journal 99: 933-939.
- Post JC, Melendez ME, Hershey DN, Hakim A (2003) Lessons learned from a successful MEDRETE in El Salvador. Mil Med 168: 287-292.
- Sareen H, Shoaf KI (2000) Impact of the 1994 Northridge earthquake on the utilization and difficulties associated with prescription medications and health aids. Prehosp Disaster Med 15: 173-180.
- Bloem CM, Miller AC (2013) Disasters and women's health: Reflections from the 2010 earthquake in Haiti. Prehospital and Disaster Medicine 28: 150-154.
- Imamura CK, Ueno NT (2011) How can we address cancer care after a natural disaster? Nature Reviews Clinical Oncology 8: 387-388.
- Krousel-Wood MA (2009) Moving beyond the katrina crisis: from danger to opportunity overview of key lessons learned for better disaster preparedness from the american journal of the medicine sciences third post-katrina anniversary symposium issue. Ochsner J 9: 60-62.
- Lach HW, Langan JC, James DC (2005) Disaster planning: are gerontological nurses prepared? Journal of gerontological nursing 31: 21-27.
- Banks L (2013) Caring for elderly adults during disasters: improving health outcomes and recovery. Southern medical journal 106: 94-98.
- Foster M, Brice JH, Shofer F, Principe S, Dewalt D, et al. (2011) Personal disaster preparedness of dialysis patients in North Carolina. Clin J Am Soc Nephrol 6: 2478-2484.
- Millin MG, Jenkins JL, Kirsch T (2006) A comparative analysis of two external health care disaster responses following Hurricane Katrina. Prehospital Emergency Care 10: 451-456.
- Jenkins JL, McCarthy M, Kelen G, Sauer LM, Kirsch T (2009b) Changes needed in the care for sheltered persons: a multistate analysis from Hurricane Katrina. American journal of disaster medicine 4: 101-106.
- Tanaka S (2013) Issues in the support and disaster preparedness of severely disabled children in affected areas. Brain & development 35: 209-213.
- Mace SE, Sharieff G, Bern A, Benjamin L, Burbulys D, et al. (2010) Pediatric issues in disaster management, part 3: special healthcare needs patients and mental health issues. American journal of disaster medicine 5: 261-274.
- Sakashita K, Matthews WJ, Yamamoto LG (2013) Disaster preparedness for technology and electricity-dependent children and youth with special health care needs. Clinical pediatrics 52: 549-556.
- Andersson HC, Narumanchi TC, Cunningham A, Bowdish B, Thoene J (2006) Genetic/metabolic health care delivery during and after hurricanes Katrina and Rita. Mol Genet Metab 88: 3-6.
- Fung OW, Loke AY (2010) Disaster preparedness of families with young children in Hong Kong. Scand J Public Health 38: 880-888.
- Mori K, Ugai K, Nonami Y, Kirimura T, Kondo C, et al. (2007) Health Needs of Patients With Chronic Diseases Who Lived Through the Great Hanshin Earthquake. Disaster Management and Response 5: 8-13.
- Lamb KV, O'Brien C, Fenza PJ (2008) Elders at risk during disasters. Home healthcare nurse 26: 30-38; quiz 39-3840.
- Nagamatsu S, Maekawa T, Ujike Y, Hashimoto S, Fuke N, et al. (2011) The earthquake and tsunami--observations by Japanese physicians since the 11 March catastrophe. Crit Care 15: 167.
- Connelly M (2006) IMERT deployment to Baton Rouge, Louisiana in response to Hurricane Katrina, September 2005. Disaster Manag Response 4: 4-11.
- Sharma AJ, Weiss EC, Young SL, Stephens K, Ratard R, et al. (2008) Chronic disease and related conditions at emergency treatment facilities in the New Orleans area after Hurricane Katrina. Disaster Med Public Health Prep 2: 27-32.
- Nufer KE, Wilson-Ramirez G, Shah MB, Hughes CE, Crandall CS (2006) Analysis of patients treated during four Disaster Medical Assistance Team deployments. J Emerg Med 30: 183-187.
- North CS, King RV, Fowler RL, Polatin P, Smith RP, et al. (2008) Psychiatric disorders among transported Hurricane evacuees: Acute-phase findings in a large receiving shelter site. Psychiatric Annals 38: 104-113.
- Krol DM, Redlener M, Shapiro A, Wajnberg A (2007) A mobile medical care approach targeting underserved populations in post-Hurricane Katrina Mississippi. Journal of health care for the poor and underserved 18: 331-340.
- Broz D, Levin EC, Mucha AP, Pelzel D, Wong W, et al. (2009) Lessons learned from Chicago's emergency response to mass evacuations caused by Hurricane Katrina. American Journal of Public Health 99: 1496-1504.
- Gnauck KA, Nufer KE, LaValley JM, Crandall CS, Craig FW, et al. (2007) Do pediatric and adult disaster victims differ? A descriptive analysis of clinical encounters from four natural disaster DMAT deployments. Prehospital and disaster medicine : the official journal of the National Association of EMS Physicians and the World Association for Emergency and Disaster Medicine in association with the Acute Care Foundation 22: 67-73.
- Cookson ST, Soetebier K, Murray EL, Fajardo GC, Hanzlick R, et al. (2008) Internet-based morbidity and mortality surveillance among Hurricane Katrina evacuees in Georgia. Prev Chronic Dis 5: A133.
- Nufer KE, Wilson-Ramirez G (2004) A comparison of patient needs following two hurricanes. Prehospital and disaster medicine : the official journal of the National Association of EMS Physicians and the World Association for Emergency and Disaster Medicine in association with the Acute Care Foundation 19: 146-149.
- Nufer KE, Wilson-Ramirez G, Crandall CS (2003) Different medical needs between hurricane and flood victims. Wilderness and Environmental Medicine 14: 89-93.
- Partridge R, King K, Proano L (2006) Medical support for emergency relief workers after typhoon Sudal in Yap, Micronesia. Prehospital and disaster medicine : the official journal of the National Association of EMS Physicians and the World Association for Emergency and Disaster Medicine in association with the Acute Care Foundation 21: 215-219.
- Taylor MM, Stokes WS, Bajuscak R, Serdula M, Siegel KL, et al. (2007) Mobilizing mobile medical units for hurricane relief: The United States Public Health Service and Broward County Health Department response to hurricane Wilma, Broward County, Florida. Journal of Public Health Management and Practice 13: 447-452.
- Noe RS, Schnall AH, Wolkin AF, Podgornik MN, Wood AD, et al. (2013) Disaster-related injuries and illnesses treated by American Red Cross disaster health services during Hurricanes Gustav and Ike. Southern medical journal 106: 102-108.
- Krieg CM, Gardemann J (2009) A record of morbidity and medical request profiles in international humanitarian aid, taking the earthquake in Bam in Iran in 2003 as an example. Journal of Public Health 17: 97-106.
- Kleinpeter MA, Norman LD, Krane NK (2006a) Dialysis services in the hurricane-affected areas in 2005: lessons learned. Am J Med Sci 332: 259-263.
- Arrieta MI, Foreman RD, Crook ED, Icenogle ML (2008) Insuring continuity of care for chronic disease patients after a disaster: key preparedness elements. The American Journal of the Medical Sciences 336: 128-133.
- Heslin KC, Gin JL, Afable MK, Ricci K, Dobalian A (2013) Personal medication preparedness among veteran and nonveteran men and women in the california population. Prehosp Disaster Med 28: 359-366.
- Adhikari A, Biswas S, Gupta RK (2011) A study on habit of preservation of prescriptions by pregnant women in India. Nepal Med Coll J 13: 17-19.
- Tomio J, Sato H, Mizumura H (2012) Disparity in disaster preparedness among rheumatoid arthritis patients with various general health, functional, and disability conditions. Environ Health Prev Med 17: 322-331.
- Bamrah S, Mbithi A, Mermin JH, Boo T, Bunnell RE, et al. (2013) The impact of post-election violence on HIV and other clinical services and on mental health-Kenya, 2008. Prehosp Disaster Med 28: 43-51.
- Kishimoto M, Noda M (2013) Diabetes care: After the Great East Japan Earthquake. Journal of Diabetes Investigation 4: 97-102.
- Cross AR (2013) Get a survival kit.
- Blackpool (2011) Green Bag campaign urges patients to take their own medicines when admitted into Blackpool hospital.: NHS Foundation Trust.
- Feret B, Bratberg J (2008) Pharmacist-based intervention to prepare residents of assisted-living facilities for emergencies. J Am Pharm Assoc (2003) 48: 780-783.
- Velazquez L, Dallas S, Rose L, Evans KS, Saville R, et al. (2006) A PHS pharmacist team's response to Hurricane Katrina. Am J Health Syst Pharm 63: 1332-1335.
- Howe E, Victor D, Price EG (2008) Chief complaints, diagnoses, and medications prescribed seven weeks post-Katrina in New Orleans. Prehosp Disaster Med 23: 41-47.
- CDC Emergency Preparedness and You. CDC.
- Allweiss P, Albright A (2011) Diabetes, disasters and decisions. Diabetes Management 1: 369-377.
- Ford ES, Mokdad AH, Link MW, Garvin WS, McGuire LC, et al. (2006) Chronic disease in health emergencies: in the eye of the hurricane. Prev Chronic Dis 3: A46.
- Davis MV, MacDonald PD, Cline JS, Baker EL (2007) Evaluation of public health response to hurricanes finds North Carolina better prepared for public health emergencies. Public health reports (Washington, DC: 1974) 122: 17-26.
- Frumkin H (2011) Bumps on the road to preparedness. Am J Prev Med 40: 272-273.
- Ablah E, Konda K, Kelley CL (2009) Factors predicting individual emergency preparedness: A multi-state analysis of 2006 BRFSS data. Biosecurity and Bioterrorism 7: 317-330.
- Islam T, Muntner P, Webber LS, Morisky DE, Krousel-Wood MA (2008) Cohort study of medication adherence in older adults (CoSMO): extended effects of Hurricane Katrina on medication adherence among older adults. Am J Med Sci 336: 105-110.

Leave a Comment
You must be logged in to post a comment.